Results from a subset analysis of the ABRE study have shown that patients in three out of the six World Health Organisation (WHO) body mass index (BMI) groups—‘pre-obesity’, ‘obesity class I’ and ‘obesity class II’—trended towards higher 36-month patency rates compared with the ‘normal weight’ group.
Erin Murphy (Atrium Health Sanger Heart and Vascular Institute, Charlotte, USA) shared this finding at the 2024 American Vein and Lymphatic Society (AVLS) annual congress (10–13 October, Chicago, USA), noting that further research on the topic is needed.
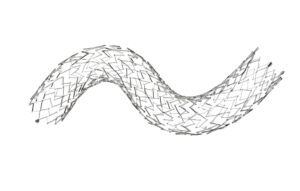
The ABRE study was designed to evaluate the safety and efficacy of the Abre venous self-expanding stent system (Medtronic) in patients with symptomatic iliofemoral venous outflow obstruction. A total of 200 patients with an average age of 51.5 years, average BMI of 29.5 and 66.5% of whom were female, were enrolled across 24 global study sites and followed for 36 months.
In her presentation at AVLS 2024—which earned the first-place Best in Show award at the meeting—Murphy detailed that the ABRE subanalysis sought to assess the impact of BMI on post-iliac vein stenting outcomes. Historically, she noted, obesity has been viewed as a potential hindrance to venous stenting, with expectations of poorer patient outcomes due to higher comorbidity risks.
For the subanalysis, patients were categorised by the six WHO BMI groups: ‘underweight’ (four patients; 2%), ‘normal weight’ (55 patients; 27%), ‘pre-obesity’ (50 patients; 25%), ‘obesity class I’ (51 patients; 26%), ‘obesity class II’ (22 patients; 11%), and ‘obesity class III’ (18 patients; 9%).
Murphy reported at AVLS 2024 that, with regard to revised venous clinical severity score (rVCSS) outcomes, the ‘pre-obesity’, ‘obesity class I’, ‘obesity class II’, and ‘obesity class III’ groups showed increasingly higher baseline scores compared to ‘underweight’ and ‘normal weight’ patients. After six months, the presenter added, improvement in rVCSS was constant across all BMI groups except for ‘underweight’.
Murphy also shared quality-of-life (QoL) results. The presenter detailed that, as BMI increases, the baseline VEINES-QoL scores worsen and that improvement in VEINES-QoL at six months is constant across all BMI groups except for ‘underweight’. BMI was not found to be a factor in VEINES-QoL change from baseline to six months, she continued.
Regarding primary patency, Murphy relayed that the ‘pre-obesity’, ‘obesity class I’, and ‘obesity class II’ groups “paradoxically” trended towards higher patency rates at month 36 compared to the ‘normal weight’ group. However, the presenter stressed that the 95% confidence intervals overlapped for all three groups and that the subgroups are small.
Finally, Murphy added that the ‘obesity class III’ group (BMI >40) had the lowest 36-month patency—which she said indicates potential higher risk in this group independent of disease cohort—and that there was no significant difference in underlying disease cohort across the BMI categories.








