Should interventional radiologists up-skill to perform emergency stroke thrombectomy and help deliver stroke services? And if they did, would the increase in the number of physicians who can offer thrombectomy be essential in delivering a round-the-clock, modern stroke intervention programme? A consensus on the rigorous training needed for timely salvage of compromised brain tissue still remains an important, thorny, and politically charged issue. Interventional News finds out more…
“Interventional radiologists have the training to properly select patients for endovascular stroke treatment, the technical skills to perform intra-arterial stroke interventions, and the clinical knowledge to manage these patients. Since they have this intensive training in the clinical management of patients, image-guided endovascular procedures, and the ability to work as part of structured, multispecialty care teams, they provide excellent care to patients with acute ischaemic stroke, with good patient outcomes,” Martin Radvany, chief, Interventional Neuroradiology, University of Arkansas for Medical Sciences, Little Rock, USA, told Interventional News.
Radvany, who is a coordinator of the Society of Interventional Radiology (SIR) Stroke Course, and many other physicians, believe that more interventional radiologists should become part of comprehensive stroke teams. “Rapid access to stroke centres that offer thrombectomy saves lives and reduces disability after stroke, but many hospitals do not have this important capability due to a need for appropriately trained specialists. Time is of the essence in caring for stroke patients, so if more hospitals can be properly staffed, we can avoid transferring patients and delaying treatment. This will save lives and prevent long-term disability. Interventional radiologists are already present in most community hospitals and are currently providing care for stroke patients at some hospitals, either where neurointerventional physicians are not available, or where they have partnered with neurointerventional physicians to provide 24/7 coverage. We need to support these existing programmes and encourage establishment of new ones,” he says.
There is, however, the matter of additional training. “Interventional radiologists can help provide endovascular thrombectomy locally and 24/7, but require additional training to do so. SIR is currently revising its stroke training guidelines. Interventional radiologists need to be expert in patient selection and endovascular treatment, and must track outcomes to be certain that care meets national and international benchmarks,” cautions David Sacks, an interventional radiologist at Tower Health System in West Reading, USA. Sacks is a past president of SIR and is current president of the Intersocietal Accreditation Commission (IAC) Carotid Stenting division.”
In the landscape of current stroke care, there are many recent developments that will have enduring effects on patient care. First, a major new recommendation from the most recent update to US ischaemic stroke guidelines released by the American Heart Association and American Stroke Association in February increases the time window for mechanical thrombectomy to be offered to 24 hours for selected acute ischaemic stroke patients. The new guideline, based on the most recent evidence available, recommends that large vessel strokes can safely be treated with mechanical thrombectomy up to 16 hours after a stroke, in selected patients. Further, under certain conditions and based on advanced brain imaging and key inclusion criteria, some patients may have up to 24 hours for treatment with mechanical thrombectomy, the guidelines state.

The previous time limit was six hours. It is widely believed that this new recommendation will likely result in more patients becoming eligible for thrombectomy since more patients will be treated based on clinical presentation rather than a time cut-off alone. Following from this, the US FDA has also expanded the treatment window for the use of clot retrieval devices in certain stroke patients.
But perhaps the most important development of all is that in 2018, large vessel embolectomy undeniably has the backing of the highest quality of evidence and represents the greatest advance in acute stroke management in a few decades. It is
recognised as a game-changer and is the new standard of care therapy for stroke patients. This has created a number of profound challenges internationally as politicians, hospital administrators, patient advocacy groups and stroke care providers are demanding that endovascular stroke treatment be incorporated into practice (effective at once), prompting careful national examinations of existing stroke services and analysis of how a comprehensive roll-out of stroke thrombectomy can be achieved.
Klaus Hausegger, head of Department of Diagnostic and Interventional Radiology, Klagenfurt State Hospital, Austria, and editor-in-chief of CardioVascular and Interventional Radiology (CVIR), comments: “Within a very short time mechanical thrombectomy has become the first-line treatment for patients with acute ischaemic stroke due to large vessel occlusion in the cerebral circulation. Very recently, two randomised trials (DAWN and DEFUSE 3 trials, both published in the New England Journal of Medicine in 2018) have shown that the time window can even be extended up to 24 hours, provided that the infarct size is still limited (as shown by multiparametric imaging) and patients have
a disproportionately high National Institutes of Health (NIH) stroke score. This means that even more stroke patients are
eligible for mechanical thrombectomy, and as a consequence, more dedicated interventionalists are required to provide
a full 24/7 service through the year. While interventional radiologists have the appropriate skills to contribute significantly to this service, those who are not experienced in neurovascular procedures should undergo rigorous training before they enter the field of endovascular stroke treatment. It is my sincere hope that a training programme specifically designed for interventional radiologists will be set up soon throughout Europe.”
Other countries, like Australia, are experiencing a similar demand for adequately trained practitioners. Gerard Goh, consultant interventional and diagnostic radiologist, The Alfred Hospital, acting head of Interventional Radiology and president of the Interventional Radiology Society of Australasia (IRSA) told Interventional News, “In addition to the several landmark papers that have demonstrated the significant benefits of stroke thrombectomy over conventional systemic anticoagulation in certain patients, advances in diagnostic imaging and the creation of dedicated stroke referral pathways are allowing patients to be rapidly assessed and referred for treatment within a time window where intervention can make a difference to outcomes. This has led to a surge in demand for adequately trained practitioners to perform stroke thombectomy.”
In January this year, there was new UK guidance released on training interventional radiologists to speed up the roll out of stroke thrombectomy services. A press release on the issue notes: “Emergency mechanical thrombectomy dramatically increases a stroke patient’s chance of a full recovery. The UK does not have enough skilled doctors to provide the procedure. NHS England plans to roll out the technique nationally, but will need at least another 50 extra specially trained radiologists.” The guidance was produced by The Royal College of Radiologists, the British Society of Interventional Radiology, the British Society of Neuroradiologists and the UK Neurointerventional Group.
The crux: “to combat a UK-wide shortage of interventional neuroradiologists—who normally perform stroke thrombectomy the umbrella group is encouraging hospitals to support existing
interventional radiologists to train in the new technique.”
Trevor Cleveland, president of the British Society of Interventional Radiology, said: “NHS England hopes that around 8,000 patients every year will be able to benefit from stroke thrombectomy, however, currently only a few hundred do so because we need more trained doctors. Training enough radiologists to carry out this specific life-changing technique will not happen overnight, however, we hope to encourage and support clinicians and hospitals to invest their time and expertise to make the promised roll out of stroke thrombectomy services a reality.”

However, the success of stroke thrombectomy is undeniably dependent on multiple factors, one of which is the training and expertise of the interventionalist delivering the care. And, the training required to perform stroke thrombectomy safely and expertly is one of the more controversial aspects of interventional radiologists performing this therapy.
Patrick A Brouwer, neurointerventionalist, Karolinska University Hospital, Stockholm, Sweden, general-secretary of the European Society for Minimally Invasive Neurological Therapy (ESMINT) and Board member of the World Federation of Interventional and Therapeutic Neuroradiology (WFITN) notes: “Anyone with proper training (as described in the consensus document of 12 international neurointerventional societies worldwide and published in three journals) is welcome to help out.”
The consensus document Brouwer points to is a paper published in October 2016 titled “Training guidelines for endovascular ischemic stroke intervention: an international multi-society consensus document”.
The purpose of the document is to “define what constitutes adequate training for physicians who can provide endovascular treatment for acute ischaemic stroke patients” note the authors and the paper sets out the training requirements, maintenance of physician qualifications and hospital requirement needed to offer this treatment. The paper summarises: “We believe that a neuroscience background, dedicated neurointerventional training, and stringent peer review and quality assurance processes are critical to ensuring the best possible patient outcomes. Well trained neurointerventionalists are a critical component of an organised and efficient team needed to deliver clinically effective mechanical thrombectomy for acute ischaemic stroke patients.”

Radvany notes: “As with any procedure, if the individuals performing the procedure are not appropriately trained there can be complications. Inadequate training would be a potential pitfall of interventional radiologists performing stroke intervention. The appropriate technical training can be ensured by integrating the training into the interventional radiology residency/fellowship pathway. SIR has created a course that provides the cognitive continuing medical education. Accredited training programmes would be expected to offer appropriate training and thus reduce the risk of harm to patients”.
While many interventional neuroradiologists do not support the idea of interventional radiologists being involved in the offering of stroke thrombectomy, there are several prominent interventional neuroradiologists, says Radvany, “such as Mary Lee Jensen (University of Virginia, Charlottesville) and Joan Wojack (Acadiana Radiology Group, Lafayette) as well neurosurgeon, Adnan Siddiqui (State University of New York at Buffalo), who support interventional radiologists participating in stroke care. I believe these leaders can help persuade the others,” he states.
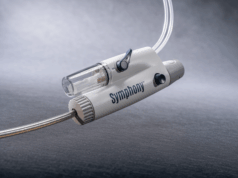
Goh returns to the importance of training: “It is important that interventional radiologists who wish to provide stroke thrombectomy be sufficiently trained and skilled. They need to be aware that the techniques of stroke thrombectomy are different to peripheral thrombectomy, although this basic skill set provides a great foundation for interventional radiologists to up-skill. There are certain important technical aspects when working in the cerebral space that are similar, but also different to, carotid interventions. Many of the catheters, sheaths, wires and devices are different to those commonly used in the peripheral space.
“In addition, there are several other factors when treating patients with stroke that interventional radiologists need to be aware of and involved with. These include the diagnostic imaging aspects of stroke including CT perfusion imaging and MRI; establishing rapid and efficient stroke care pathways in conjunction with stroke physicians; and to be trained and skilled with the technical aspects of stroke thrombectomy. I would encourage all interventional radiologists who are interested in performing stroke thrombectomy to seek training and upskilling in collaboration with interventional neuroradiologists to help provide a comprehensive service to all patients,” he says.