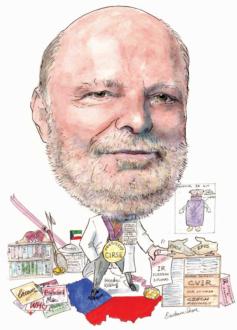
Jan Peregrin, CIRSE president 2009, told Interventional News that the miniaturisation of interventional devices hold great promise and that this will allow many clinical possibilities. He spoke of his pride at the very first diagnostic angiography procedure that he performed, how children can make for challenging patients and his enjoyment of bands and artists such as Cream, Joe Cocker, Fleetwood Mac, The Who, and others
What is that fascinates you about interventional radiology even today?
Even after many years in the field, I am still continually impressed by the permanent advances that IR makes. It is an ever-changing field that is constantly offering new methods, new devices and new possibilities: a kind of “never-ending story” of medical advancement. Techniques continually emerge, then disappear for a while, and then re-emerge in a new form, and it is very exciting to watch this progression.
You have said that Alfred Belan was a mentor… What was his philosophy, and what advice of his do you carry with you still?
I came to the department just when coronary angiography was first being implemented. I was present for the first peripheral angioplasty in Czechoslovakia, and the first coronary angiography as well. We did not have very much support from surgeons, as they did not believe that this method could work. What I learned from Belan was: “If you really want to achieve something, if you try hard enough and long enough it is almost always possible.” I think this sums up the philosophy of most interventional radiologists—it is certainly something that I constantly remind myself of.
Which innovation in IR has shaped your career the most?
There have been many innovations that have impacted on my work, such as the rapid and continuous evolution of diagnosis and treatment of occlusive arterial disease; PTA; thrombolysis; stents; covered stents; stent-grafts; drug-eluting stents and balloons. We cannot even begin to imagine what the future will bring.
However, if I had to pick one, it would have to be angioplasty—specifically, my first angioplasties, which suddenly opened my eyes to the fact that radiology is not just a diagnostic, but also a therapeutic specialty. I, and we, suddenly had a tool in our hand that was capable of opening arteries and keeping them open for a surprisingly long time.
Could you describe a memorable case you treated when “IR came to the rescue”?
We once had a strange case of post-bioptic kidney bleeding, where none of the clinicians involved could locate the source of bleeding. The surgeon involved was prepared to remove the kidney, but just in time, it was discovered that the source was a punctured inter-costal artery, which we IRs were able to embolize, saving the patient’s kidney.
More recently, we had a patient who was a kidney recipient from a living donor (his father). A few days following the procedure, the kidney just was not functioning, with normal arterial perfusion, without collecting system dilatation. Based on past experience, I performed a nephrostomy and found occlusion of the urethra close to the bladder. I managed to open the occlusion by means of a balloon, and the kidney began to work. Seven months on, the patient is showing normal graft function without any need for a catheter.
Which developing techniques and technologies in IR are you watching closely for the future?
The miniaturisation of interventional devices holds great promise, and will allow many clinical possibilities. I am looking forward to the day that almost every procedure can be done percutaneously. Based on that, it may be possible to implement one-day procedures, so that the patients need not stay in hospital at all.
As president of CIRSE 2009, could you comment on the importance of Skill Certificate based on the European IR curriculum?
I share the opinions of my predecessor, Jim Reekers that having this certificate will mean that CIRSE will no longer be a group who has IR as a hobby, but rather, IR will be a recognised subspecialty with its own curriculum and a European diploma. The holder of this diploma will be recognised all over Europe as qualified IR, which is a huge move forward.
What do you think the big areas of growth in interventional radiology are?
Areas that I feel sure IR is going to make huge advances in are interventional oncology, gene therapy and diabetic foot treatment. These are the subspecialties that are already showing great promise, and ones which are sure to become even more important as they mature.
Could you briefly trace the way interventional radiology has developed in the Czech Republic from when you started out until today?
When I started in IR it was just a part of diagnostic radiology—nobody specialised in interventional procedures. Diagnostic angiography and catheterisation slowly developed into vascular interventions (mainly angioplasty). In the late 80s, we started to perform non-vascular procedures as well (nephrostomy, biliary drainage), and in recent years, interventional oncology procedures as well. In my country, IR is quite well organised. We hold two meetings a year— one dedicated to angioplasty and stenting; and one to other interventional procedures. Our group is trying to be active within CIRSE as well.
Radiographers and IRs are great allies… can you expand on the importance of this relationship?
We all know that radiographers are indispensable allies in our everyday practice and if we want to increase the quality of our work, we have to increase the quality of our radiographers (and nurses) as well. They should not be just passive helpers, but active members of the IR team.
As someone with a special interest in renal artery PTA, given the current trial data, what do you think lies in store for the procedure?
One of the major trials that is going ahead in this field is ASTRAL. The outcomes thus far tell us “If you are not sure if the patient can benefit from PTRA or if he/she could be kept well on conservative therapy, do not do PTRA. Moreover, indicate only patients with really significant stenosis or/and progressive deterioration of kidney function. What it certainly does not advise is to deny PTRA treatment to patients who are suitable candidates. I think it is important for everyone to be fully aware of the need for proper patient selection. When used appropriately, PTRA has very good outcomes.
What are some of the challenges for IRs of performing renal artery PTA in children and in transplant patients?
Children can be challenging patients: it is necessary to use small catheters (which are not in proportion to their bodies), and stents are usually difficult to use, as they will not grow with the child. Their size might not be appropriate, there are difficulties calculating the amount of contrast medium needed, and there is a tendency to spasm. Furthermore, lesions in children are usually not in main stem of renal artery but in peripheral branches whcih makes the procedure even more challenging.
Kidney transplant patients too bring their own specific challenges: they are usually more sensitive to ischaemia and contrast medium load. As these patients have just a single functional organ, failure can have the serious consequence of leaving the patient completely without kidney function.
Radiation protection is a big issue in IR… What is your advice to youngsters in the field?
In order to reduce unnecessary radiation exposure in both patients and practitioners, one should do indicated procedures only; proper coning is essential; do not zoom; ask the radiographer to give you a notice if something is incorrect (like too large a distance of an image intensifier from the patient). Always wear not only a lead apron, but a lead collar and protective glasses as well.
Can you share some of the proudest moments in your career?
I recall clearly how proud I was when I did my first diagnostic angiography—I accomplished the whole procedure myself from start to finish, including femoral artery puncture and catheter insertion. The same happened with my first ever peripheral angioplasty—another wonderful moment in my career.
Being named professor of Radiology was, without a doubt, a major highlight, but the proudest moment of all was when I was elected CIRSE president.
Can you identify three key areas that the IR field must address in order to move forward?
If the discipline is to move forward, IRs must insist on being more clinically involved, and must take full responsibility for the patient before and after procedures. As part of this process, it is necessary that we gain access to our own patients and, equally importantly, our own beds.
Outside of medicine, could you tell us some of the bands and science fiction or fantasy novels that you enjoy?
I enjoy bands and artists such as Cream and Eric Clapton, blues bands (preferably British blues), Joe Cocker, Fleetwood Mac, King Crimson, Rod Stewart, The Who and ZZ Top.
I am a big fan of sci-fi books, most notably Ray Bradbury’s Martian Chronicles, JRR Tolkien’s
Hobbit and Lord of the Rings, Stanislaw Lem’s
Solaris, and the works of Dan Simmons, Philip K Dick, and Orson Scott Card. However, also deserving mention is a pioneer of fantasy books, Edgar Rice Burroughs, who brought us Tarzan and the excellent Barsoom series.
Factfile
Education
1969–75 Faculty of Medicine, Charles University, Hradec Králové (MD degree)
1978 First degree specialisation in Diagnostic Radiology
1981 PhD in Medical Sciences
1982 Second degree specialisation in Diagnostic Radiology
1998 Associate professor, Third Medical Faculty, Charles University, Prague
2008 Full professor, Medical Faculty Hradec Králové, Charles University
Employment
– 1975–84
Department of Radiology, Research Center of Cardiovascular Disease, Institute for Clinical and Experimental Medicine, Prague Czechoslovakia Assistant Professor, Department of Radiology, Faculty of Medicine, University of Kuwait, Kuwait Division of Interventional Radiology, Department of Radiology, Institute for Clinical and Experimental Medicine, Prague, Czechoslovakia
– 1991–present
Head, Department of Diagnostic and Interventional Radiology, Institute for Clinical and Experimental Medicine, Prague, Czech Republic
Scientific background
Member of the Czech Radiological Society Executive Committee
Past president of the Society of Interventional Radiology of the Czech Republic
Author and co-author of more than 170 scientific and educational papers
Local chairman of the 1st–8th workshops of Interventional Radiology, Prague, Czech Republic (1994–2002)
Chairman of CIRSE 99 Prague
CIRSE programme committee member 1997–9
CIRSE executive committee member since 1999, Board member since 2005
CIRSE programme chairman 2001 and 2002
CIRSE Treasurer 2005–2007
CIRSE vice-president 2007–2009
CIRSE President 2009
Member of CVIR Editorial Board
Member of Cor et Vasa Editorial Board
Member of Česká Radiologie (Czech Radiology) Editorial Board













