The evolution of embolization over the past decade has been remarkable and it has fundamentally changed our field, James B Spies, professor of Radiology, Georgetown University School of Medicine, Washington DC, USA, and the incoming president of the Society of Interventional Radiology in 2014, tells Interventional News. He also highlights the importance of multidisciplinary treatment and multidisciplinary research because “we cannot carry out and ensure quality care in a vacuum”
What drew you to medicine and interventional radiology?
I chose medicine after taking a physiology class in high school, during which I became fascinated with how the body works. I did not really know about interventional radiology until I was an intern. The interventionist in that hospital, John Wok, was doing amazing things even in those days (1980). I was finally sold on it after spending time on interventional at University of California, San Francisco (UCSF) during residency with Ernest Ring and Bob Kerlan. What a great set of role models for our field!
Which procedures in interventional radiology have shaped your career?
Well, since I do mostly uterine embolization, both in clinical practice and in research, that clearly is the first choice. I have loved being a part of the growth of this treatment. It works really well, has a great patient population to engage with and is fun. I would say my interests have broadened over the years and now I am excited about all types of embolization. This whole field has “grown up” during my tenure in medicine and it has been wonderful to be a part of it.
Who were your mentors and what wisdom did they impart to you?
Well my first mentors in the field were Ernest Ring and Bob Kerlan, as well as other members of the UCSF group like Anton Pogany. My good friend, Dana Burke, was a year ahead of me in training and he was also a big influence as a friend, mentor and partner. Bob Rosen, who trained me during fellowship, was the other big influence on me early on. He had a great low-key style, outstanding skills and he never got ruffled. Just the type of mentor every fellow needs!
You have contributed significantly to building the evidence base for uterine artery embolization. What clinical questions regarding the procedure would you like to see answered?
The biggest questions relate to those women who would like to become pregnant. When is it better to do myomectomy and when should uterine artery embolization be the first choice? This depends on many factors, including patient age, extent of fibroids, fitness for surgery, prior treatments and others. So it is not a one-size-fits-all answer and we have many gaps in our knowledge.
Could you describe a memorable case?
We have always been careful regarding fertility after uterine artery embolization, but I had a patient who had been trying to get pregnant for nearly 16 years. She had developed fibroids early and had undergone three prior myomectomies by the time I saw her. She had never been able to become pregnant, despite trying after those surgeries. She came to me a week before a hysterectomy was scheduled for her. She was 39 at the time. We did the uterine artery embolization without problem and a hysterectomy was avoided. Eighteen months later she became pregnant and delivered a healthy baby boy. She was the most grateful patient I have ever had and it reminded me that general rules have many exceptions.
What is your message to young interventional radiologists about the available embolic agents for uterine artery embolization?
This is one area in which we have substantial comparative data. Several investigators have completed randomised trials comparing these products and our knowledge of them is very strong. Tris-acryl gelatin microspheres (Embospheres) and particle poly vinyl alcohol (Contour) have been studied in comparative trials and are very effective for uterine artery embolization. Spherical poly vinyl alcohol (Contour SE) is not nearly as effective as these other two products and should not be used. There are two additional products: spherical acrylamido poly vinyl alcohol microspheres (Bead Block) and polyzene F-coated poly vinyl alcohol hydrogel spheres (Embozene), for which there is some research to suggest that these are also effective and there are ongoing investigations of these latter products to assess outcomes.
As the incoming SIR President, what are your goals for the society in your presidential term?
We are very focused on two mid-term goals. The first is the successful implementation of the Interventional Radiology/Diagnostic Radiology pathway for training. This new path will continue to ensure our diagnostic imaging skillset, but broaden and deepen both our technical and clinical skills in caring for patients undergoing interventional therapies. This is a huge step forward. The second goal is to advance our programme in quality and safety. The main vehicle for this effort is the ongoing development of a registry based on structured reporting of certain key procedures. We are developing quality metrics related to those procedures, and these will be used for quality reporting purposes under the evolving healthcare reform programme. Our goal here is to provide our members with the tools they need to assess their own practice and to participate in national efforts to improve patient care and outcomes.
In today’s healthcare landscape, how important is collaborative and multidisciplinary research for interventional radiologists?
Much of what we do these days is done in the context of multidisciplinary efforts to manage complex medical conditions, whether it is cancer, liver failure or other similar serious illnesses. We cannot carry out and ensure quality care in a vacuum. Quality research is the same—interdisciplinary, which provides for a broader context in any project and ensures a wider audience for the results.
In your view, what are three “general medicine” concepts that interventional radiologists need to think about?
They really parallel the three phases of care—assessment at the time of consultation, care during the procedure and follow-up care and management of outcomes. First, we need to assess patients in the context of their other medical conditions, alternative therapies, and risks for sedation or the interventional procedure. We need to make a recommendation, including recommending something other than an interventional radiology procedure where appropriate, based on this holistic approach. Second, we need to use our medical knowledge to manage the patient during the procedure, particularly related to airway maintenance while providing a comfortable degree of sedation for the patient. After treatment, we need to use our clinical skills to ensure the patient has an uneventful recovery. We also need to provide the follow-up to guide transition of care back to other providers or to make recommendations for additional interventional care. In short, we need provide the continuum of care, not just the intervention. From my perspective, this is the most rewarding aspect of my practice.
What is your proudest achievement in interventional radiology?
I am most proud of the collective effort of all the investigators in our field that has resulted in the acceptance of uterine embolization as a validated treatment for women with symptomatic fibroids. This is not my accomplishment, but the work of hundreds in our field worldwide. It is one of the best examples that we have of the power of quality research to change the recommendations for care for a very large number of patients.
What developments in interventional radiology have had an impact on the specialty recently?
Broadly speaking, I think the evolution of embolization over the past decade has been remarkable and it has fundamentally changed our field. The technology has evolved remarkably and its application has been dramatically broadened.
What are your interests outside of medicine?
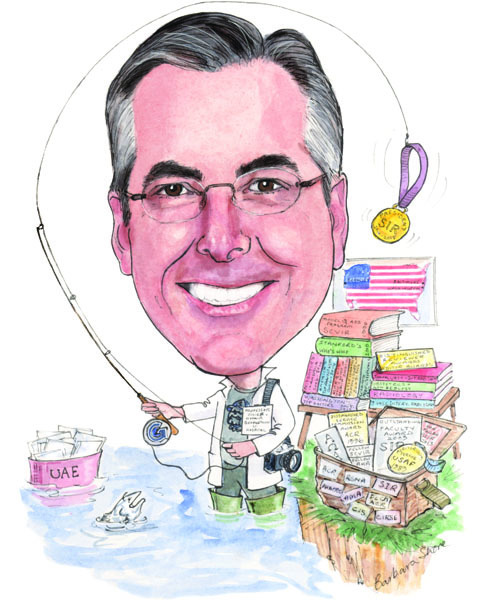
I am an avid college basketball fan and get through the winter by following the Georgetown Hoyas. I love photography and I enjoy fly fishing. I am mediocre at the former and not a great threat to the fish with the latter, but both get me away from work.
Fact file
Current appointment
Chairman, Department of Radiology
Georgetown University Hospital, Washington, USA (2005–present)
Current academic appointments
Professor of Radiology, Georgetown University School of Medicine, Washington, USA (2003–present)
Residency
University of California School of Medicine, San Francisco, USA (1981–1984)
Fellowship
New York University School of Medicine, Vascular and Interventional Radiology, New York, USA (1984–85)
Awards and honours (selected)
Distinguished Reviewer, Obstetrics and Gynecology (2009)
Distinguished Fellow, Cardiovascular and Interventional Radiology Society of Europe (2013)
Honorary Fellow, British Society of Interventional Radiology (2013)
Professional society memberships (selected)
American College of Radiology
Radiologic Society of North America (RSNA)
Society of Interventional Radiology (SIR)
American Heart Association
Cardiovascular Radiology Council
American Medical Association
Cardiovascular and Interventional Radiology Society of Europe
Professional committees
Incoming president, Society of Interventional Radiology (2014–2015)
Secretary, Society of Interventional Radiology (2012–2013)
Member, SIR Value Task Force (2011–present)
Member, Journal of Vascular and Interventional Radiology (JVIR)
Chair, Society of Interventional Radiology Evidence-based Interventional Radiology Committee (2009–2011)










