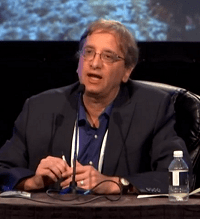
At the Society of NeuroInterventional Surgery’s 18th annual meeting (SNIS; July 26–29 2021, Colorado Springs, USA and virtual), Jeffrey Saver, professor of Neurology at the University of California, Los Angeles (UCLA) Medical Center and director of the UCLA Stroke Center (Los Angeles, USA), discussed the various ethical considerations that need to be taken into account regarding robotic applications in neuroendovascular interventions, and remote stroke care, stating that “we all need to work together to make sure patients have the best outcome”.
During a session that also saw multiple presentations demonstrating the potential benefits and new possibilities enabled by these novel technologies, Saver claimed this is an area that brings up “several unique domains of challenging bioethics”—including the ethics of remote care, the ethics of introducing new surgical techniques and training protocols, the ethics of robot-assisted procedures, and even autonomous, artificial intelligence (AI)-powered robotic systems, which are currently physician-supervised but may be unsupervised in the future.
The first specific ethical consideration Saver outlined was “compromised informed consent” on the patient’s part. He emphasised the criticality of full disclosure of the fact many of these procedures are fairly new, and, as such, there is limited evidence on both their benefits and their risks. “There is a general tendency for patients to equate newness with increased benefit—and we have to counter this tendency when we talk with them,” he added. Saver also noted that, while trust in the authority of the interventionist performing the given procedure should be encouraged, “humility”—to reflect their often-limited experience in performing these procedures compared to more traditional surgeries—is important here too.
Saver went on to state that various conflicts of interest on the physician’s side are significant too, and should be fully disclosed to the patient, with these ranging from direct financial benefits and other incentives, and brand loyalty, to the “elevated social status” of being a surgical innovator and bias towards performing a technique in which training has been invested—referring to the phenomenon of “sunk cost” here as well.
He noted that harm to the patient, including increased morbidity and mortality, is the “most important” ethical consideration that may be associated with robotic or remote procedures. “We need stringent QI [quality improvement] and reviews of every case,” Saver added. He went on to state that research burdens should not be placed disproportionately on disadvantaged or poorer communities, despite the fact that patients from these backgrounds may only gain access to advanced care by participating in innovative therapy systems—something he described as a “challenging ethical issue”—and added that these expensive technologies should not take too many resources away from proven care approaches either.
Another factor that Saver claimed is especially pertinent to remote intervention is the notion of a “diminished physician-patient relationship”, whereby the patient has reduced access to the interventionist. “We need to be sure that the interventionist maximises their availability to the patient—not just during the case, but by telemedicine pre and post if they are doing a case remotely,” he stated. Saver noted that there could be a risk for decreased empathy on the part of the physician for patients and families with whom they have never had direct contact too.
On a similar note, he alluded to the “diffusion of responsibility” that may be seen to be associated with these novel surgeries, referring to a “broader network of interdependent care” than is common in medicine. This network involves the remote interventionist, local physicians and nurses, hardware manufacturers, software coders, the AI system being deployed, and more. “We need to make sure we have an active, continuous partnership,” Saver also said.
As well as giving a nod to the more distant future in this ever-evolving space within neurosurgery—that being the ethics of fully autonomous, robotic interventionists—Saver chose to end his presentation on a more positive note. Firstly, he encouraged the attending audience to consider the future of their own patients, but also future generations of patients who, further down the line, stand to benefit from many of the innovations currently being advanced, adding that “a procedural speciality does require a little bit of risk taking”. Saver concluded his talk by addressing the need to consider the wellbeing of the physicians themselves in this debate—noting that the minimised radiation exposure and reduced lead-wearing risks that neurointerventionists may gain via robotic or remote surgical techniques are “a very important ethical goal” as well.