Six-month outcomes from the randomised RADIANCE-HTN TRIO trial, comparing endovascular ultrasound renal denervation to a sham procedure for treatment-resistant hypertension, demonstrate the additional effects of pharmacologic intervention with maintenance of a blood pressure-lowering effect of renal denervation at six months, according to investigators.
The six-month results were presented during a late-breaking trial session at the Transcatheter Cardiovascular Therapeutics annual meeting (TCT 2021; 4–6 November, Orlando USA and virtual) by Ajay Kirtane (Columbia University Irving Medical Center/NewYork-Presbyterian Hospital, New York, USA). These build upon the presentation of the trial’s two-month findings at the American College of Cardiology’s 70th Annual Scientific Session (ACC.21, 15–17 May, virtual) and also published in The Lancet.
Patients with hypertension require a multi-faceted approach for blood pressure control, Kirtane explained, detailing that in RADIANCE-HTN TRIO, patients with daytime ambulatory systolic blood pressure (dASBP) 135/85mgHg despite a fixed dose combination pill consisting of a calcium channel blocker, angiotensin receptor blocker, and thiazide diuretic, were randomised to renal denervation using the Paradise renal denervation ultrasound system (ReCor Medical, n=69) or a sham procedure (n=67).
The trial’s two-month results found that, in conjunction with the three-drug fixed-dose combination pill, renal denervation reduced dASBP by an additional 8mmHg, a 4.5mmHg greater reduction compared with a sham procedure (–8mmHg versus –3mmHg; median between-group difference–4.5mmHg; adjusted p=0.022).
During months two through five, the addition of a standardised stepped-care antihypertensive treatment (SSAHT) was recommended sequentially with the addition of spironolactone 25mg/d, bisoprolol 10mg/d, full dose of a centrally acting α2 receptor agonist, and an α1 receptor blocker if monthly measured home blood pressure was ≥135/85mmHg, with the goal of achieving blood pressure control in both groups. Adherence to prescribed medications was similar in both groups (71% for renal denervation versus 78% for sham, p=0.41).
The increase in the number of antihypertensive medications at six months following the addition of the SSAHT was 0.7±1 for renal denervation and 1.1±1.1 for sham (p=0.045). The use of aldosterone antagonists at two months was 3% for renal denervation and 11% for sham (p=0.16). At six months, the number increased in both groups but to a lesser extent in the renal denervation group (40% for renal denervation compared to 60.9% for sham, p=0.017).
The addition of the stepped care antihypertensive regimen to the initially randomised therapy further decreased blood pressures in both arms; the overall change from baseline in dASBP was -11.8±14.2mmHg in the renal denervation group versus -12.3±14.2mmHg for sham (p=0.65). Home blood pressure was lower in patients initially randomised to renal denervation when adjusted for baseline blood pressure and number of medications (-4.28mmHg, p=0.027). Safety outcomes were similar for both groups.
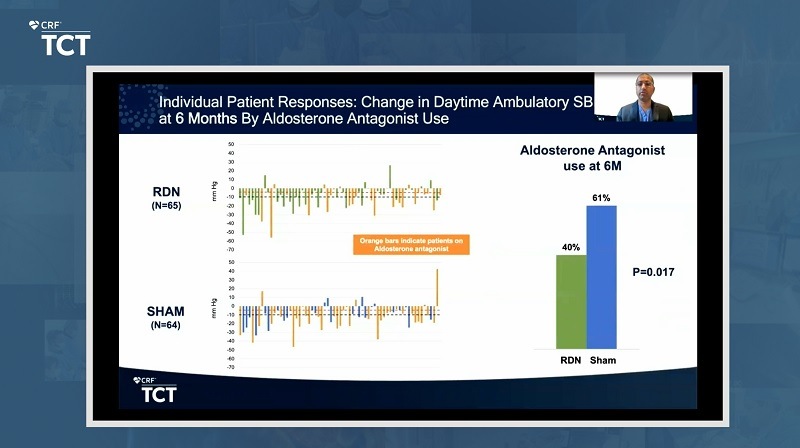 “Blood pressure reductions after renal denervation were achieved with a smaller increase in additional medications prescribed and less use of aldosterone antagonists compared with a sham procedure,” said Kirtane. “These results demonstrate the additional effects of pharmacologic intervention with maintenance of a blood pressure-lowering effect of endovascular ultrasound renal denervation at six months.”
“Blood pressure reductions after renal denervation were achieved with a smaller increase in additional medications prescribed and less use of aldosterone antagonists compared with a sham procedure,” said Kirtane. “These results demonstrate the additional effects of pharmacologic intervention with maintenance of a blood pressure-lowering effect of endovascular ultrasound renal denervation at six months.”
During a press conference in which Kirtane presented the latest findings of the study, describing them as “exploratory”, he relayed that the addition of a pharmacologic intervention led to further blood pressure reductions after renal denervation with a smaller increase in additional medications prescribed and less use of diuretics.
In ensuing discussion during the press conference, David Kandzari (Piedmont Heart Institute, Atlanta, USA) described the findings as “welcome” as they add to the totality of evidence around renal denervation. Responding to a question as to whether, given the relative differences in the reduction in blood pressure in both arms, patients would be more willing to undergo an invasive intervention for hypertension, Kandzari noted that reducing medication burden is of “increasing importance” to patients.
He added: “The opportunity to reduce the medication burden in discrete choice experiment studies is one of the key drivers of patient motivation for an alternative therapy or approach like renal denervation.
“Indeed, patients do not typically want to undergo an interventional procedure, but if there is durability with it and if there is a meaningful reduction in blood pressure, which, interestingly by patients’ criteria does not have to be that large of a reduction in blood pressure to be meaningful, and the opportunity to reduce medicines, then it is clinically important to them.”
Kandzari also referred to new data to be presented at TCT 2021, that has sought to quantify US patient preferences for considerations of interventional procedures in the treatment of high blood pressure, including treatment mode, effectiveness and risks.
Roxana Mehran (Icahn School of Medicine at Mount Sinai, New York, USA) questioned if the results demonstrate the “durability” of renal denervation, but described the study as an “exciting next step”. “To me it is opening a window,” she remarked. “Previously the doors might have been closed for renal denervation, but I think the window is opening and it may be a large one!”








