The FOXFIRE, SIRFLOX and FOXFIRE Global randomised studies evaluated the efficacy of combining first-line chemotherapy for metastatic colorectal cancer with selective internal radiotherapy (SIRT) using yttrium-90 resin microspheres (SIR-Spheres, Sirtex) in patients with liver metastases. The combined FOXFIRE analysis comprises data from the SIRFLOX study, first presented in 2015, and data from two new studies – FOXFIRE and FOXFIRE Global.
The studies were designed for prospective, combined analysis of overall survival. Data from combined analysis showed that there was no statistically significant difference between the overall survival of patients who received SIR-Spheres plus standard first-line chemotherapy and those who received chemotherapy alone. The combined analysis data were published as an abstract by the American Society of Clinical Oncology (ASCO) and will be presented at the society’s annual meeting on 5 June 2017.
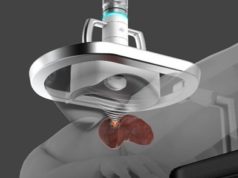
As published in the ASCO abstract, the three trials randomised (1:1) chemotherapy-naïve metastatic colorectal cancer patients (performance status 0/1) with liver metastases not suitable for curative resection/ablation. Arm A was oxaliplatin-based chemotherapy (mFOLFOX6/ OxMdG)±investigator-chosen biologically targeted agent. Arm B was the same systemic therapy (oxaliplatin dose modification)+single treatment SIRT with cycle one or two of chemotherapy.
The minimum sample size was 1,075 patients. Secondary outcomes included progression-free survival, liver-specific progression-free survival and response rate. Apart from safety, outcomes were analysed on an intention-to-treat basis using meta-analytic methods of pooled individual patient data.
Secondary analyses of data from SIRFLOX and FOXFIRE Global show a statistically significant nearly five-month improvement in median overall survival in patients with right-sided primary colon cancer favouring the SIR-Spheres plus chemotherapy arm (p=0.007). Patients in this population had a statistically significant 36% reduction in their risk of death, and lived a median of 4.9 months longer when SIR-Spheres were added to chemotherapy compared with when chemotherapy was used alone, a press release from Sirtex states. These data are expected to be presented at the World Congress of GastroIntestinal Cancers in Barcelona, Spain, in June.
Between 2006 and 2014, 1103 patients were randomised in 14 countries. The median age was 63 years; median follow-up 43.3 months. There were 844 deaths. There was no difference in overall survival (p=0.609) or progression-free survival (p= 0.108) between arms. Objective response rate (p=0.001) and liver-specific progression (p< 0.001) were significantly more favourable in arm B. Patients in arm B had higher risk of non-liver progression as first event (p<0.001). Grade three to five adverse events were more common in arm B (74%) than A (66.5%; p=0.009). In health status questionnaires, EQ-5D utility scores were not significantly different between arms at six, 12 or 24 months.
The investigators concluded that despite the higher response rates and improved liver-specific progression-free survival, the addition of SIRT to first-line oxaliplatin-fluorouracil chemotherapy for patients with liver-only and liver-dominant metastatic colorectal cancer did not improve overall survival or progression-free survival.
“While these results are not what we expected, we believe that SIR-Spheres Y-90 resin microspheres will continue to play an important role in the treatment of patients with metastatic colorectal cancer,” said Gary Donofrio, senior vice president Americas, Sirtex Medical. “We are committed to helping people with advanced colorectal cancer and look forward to additional validation of this potentially significant finding to improve survival in patients with right-sided colon cancer in the first-line setting.
“Understanding why patients with right-sided colon cancer do not respond as well to certain drug regimens is currently one of the most actively investigated and controversial conundrums in the gastrointestinal oncology field,” Donofrio continued. “We have known for several years that patients with right-sided colon cancer that metastasises generally have a poorer prognosis than those with left-sided disease. If our initial findings are confirmed, a five-month improvement in median survival in the first line setting could be seen as clinically meaningful in this difficult-to-treat population with liver metastases.”