The publication of a consensus statement from the European Society of Cardiology (ESC) Council on Hypertension and the European Association of Percutaneous Cardiovascular Interventions (EAPCI) is among the final steps in the evaluation of renal denervation as a device-based treatment for hypertension. This is according to Felix Mahfoud (Saarland University Hospital, Homburg, Germany), a member of the expert committee behind the paper, and one of the foremost investigators of the technique. He discusses patient selection and future indications for the therapy with Interventional News.
What is the background to the ESC/EAPCI consensus statement on renal denervation?
This consensus document was deemed necessary because a significant amount of new sham-controlled trial evidence has become available. In the 2018 guidelines of the ESC and the European Society of Hypertension (ESH), device-based hypertension treatment was graded with a class 3 recommendation, not to be used routinely in clinical practice. There was a sentence added to the statement that until further evidence regarding the safety and efficacy becomes available these devices should not be used outside of clinical trials.
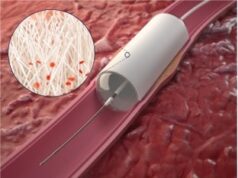
We felt it was important to re-evaluate the evidence that has aggregated after publication of the guidelines, and by now we have five sham-controlled clinical trials that have indeed proven the efficacy and safety of renal denervation in the presence and absence of antihypertensive drugs.
What have the recent trials shown and how are these reflected in the consensus statement?
We know it works in patients with and without antihypertensive medication, but this is a very broad potential patient population. We felt it is also important to provide some guidance on where denervation may be used in clinical practice and felt this should be reserved as a treatment option for patients with so-called “resistant” hypertension, meaning despite treatment with three antihypertensive drugs, they still have uncontrolled blood pressure values, as confirmed by office and ambulatory blood pressure.
Despite the fact that we have evidence that this works in a very broad potential patient population, we nailed it down, first and foremost, to patients with resistant hypertension. There is another potential indication for renal denervation and that is in patients where drugs are not tolerated, patients who are not willing or able to take antihypertensive drugs, and patients who express a preference to be treated with a device-based approach.
How significant a development is the consensus statement?
It is not the intent of the consensus statement to change people’s perception. The perception needs to be adapted according to the published trial evidence. This is really more to inform clinical practice.
What we did here is reach consensus on different statements. The challenge is who to treat within clinical practice, and this is the overall objective of such consensus statements. Which patients in which centres? How should the centres be trained? What are the potential complications of the procedure that interventionalists need to be informed about?
Are there “ideal” patients for renal denervation?
What we have to accept is that this is a treatment possibility for patients with uncontrolled blood pressure. It is not replacing drugs, it is not replacing lifestyle modification—that this is another approach available in our armamentarium to lower blood pressure. But, it is not exclusive. It is not renal denervation or nothing. Most patients we treat have undergone lifestyle modification, but it was unsuccessful. They have been treated with several drugs, are still uncontrolled and have high blood pressure and have high cardiovascular risk. In these patients it is another treatment that may bring blood pressure down.
You have studied renal denervation in great detail, how excited are you by this treatment?
We started the scientific evaluation of this approach 15 years ago. It is among the very, very few device-based treatments that has been investigated against and has beaten sham control. This is something we have to keep in mind. There has been a very rigorous evaluation of procedure, which is not available for other techniques that we are using every day. This is something we have to acknowledge, that we have a lot of clinical data, a lot of robust methodologically defined and properly designed studies conducted around the world and they have proven that this technology lowers blood pressure. You cannot question whether or not it works—it works—that is a statement, and now it is our responsibility as physicians to offer this to certain, but of course not all, patients at risk.
I am excited, of course, because it is about science, but this is probably among the last steps in the evaluation of this technology and this technique. We are working on a US Food and Drug Administration (FDA) submission so hopefully this will become available in the USA sometime soon. I think overall we are in good shape moving forward with this technology.
We are now looking into new indications such as heart failure, atrial fibrillation and ventricular tachycardia. We have registry data confirming that in those populations it is safe, and now we are heading off to new shores and among those are heart failure, certainly and arrhythmias are very interesting also.
Where are the gaps in our knowledge regarding renal denervation?
Identification of responders is the unmet need, something that we are investigating in clinical studies to get further insights, and has never become available even for antihypertensive drugs. I am not sure if we will succeed in this with renal denervation, but we are still trying.
The second question is whether or not this blood pressure lowering translates into improvements in outcomes. We know that blood pressure as LDL [low-density lipoprotein] cholesterol closely associate with cardiovascular morbidity and mortality, and when you lower blood pressure or LDL cholesterol, it is believed that it lowers morbidity and mortality too, so I am pretty confident that this will translate into improved outcomes—but it has not yet been shown.