Percutaneous microwave and cryoablation allow for repeat minimally invasive treatment of sarcoma lung metastases with mild complications, according to the conclusions of a study published in the American Journal of Roentgenology (AJR).
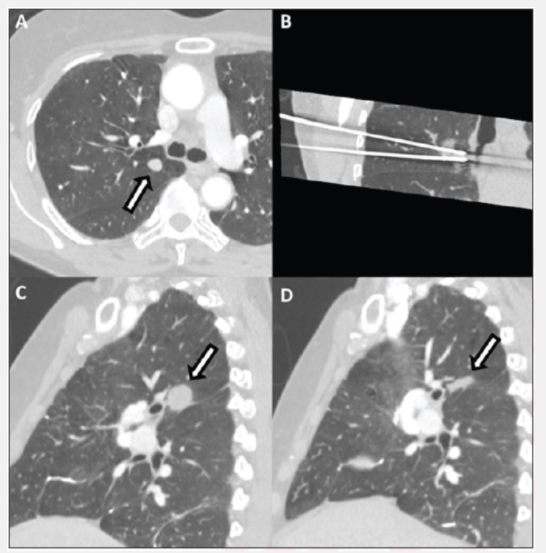
“High primary technical success, local control, and overall survival” were the supporting findings, as reported by Florian Fintelmann (Massachusetts General Hospital and Harvard Medical School, Boston, USA) and colleagues. Fintelmann and colleagues’ retrospective cohort study included 27 patients, consisting of 16 women and 11 men, with a median age of 64 years and an Eastern Co-operative Oncology Group performance score of 0–2. The patients received 39 percutaneous computed tomography (CT) guided ablation sessions (21 microwave, 18 cryoablation) with one to four sessions per patient.
CREDIT
American Roentgen Ray Society (ARRS), American Journal of Roentgenology (AJR)
USAGE RESTRICTIONS
Image may only be used with appropriate caption or cred
The sessions were to treat 65 sarcoma lung metastases (median 1 tumour per patient, range 1–12; median tumor diameter 11mm, range 5–33mm; 25% non-peripheral) from 2009 to 2021. Ablation modality complications were compared using generalised-estimating equations. Cox hazard methods were also used to evaluate ablation modality, tumour size, and location (peripheral versus non-peripheral) in relation to local tumour progression, with death as a competing risk. Overall survival was also estimated using the Kaplan-Meier method.
The median follow-up time was 23 months (range 1-102 months) and the estimated two-year microwave local control rate was 95% vs. 98% for cryoablation for tumours ≤1cm and 62% and 79% for tumours >1cm. Furthermore, decreased cumulative incidence of local progression was associated with tumour size ≤1cm. Fintelmann and colleagues also noted that ablation modality and tumour location did not affect local progression (p>0.05) and “treatment failure was low, especially for small tumours, with non life-threatening complications for tumours ≤1cm”.
Across 44% of patients, complications (≤grade 3) occurred, resulting in chest tube placement in 23% of these patients. No complications ≥grade 4 occurred and overall survival was 100%, 89%, and 82% at one, two, and three years respectively. Therefore, both percutaneous microwave and cryoablation are suited for the treatment of sarcoma lung metastases, especially in peripheral or non-peripheral tumours ≤1cm, the study’s authors conclude.









