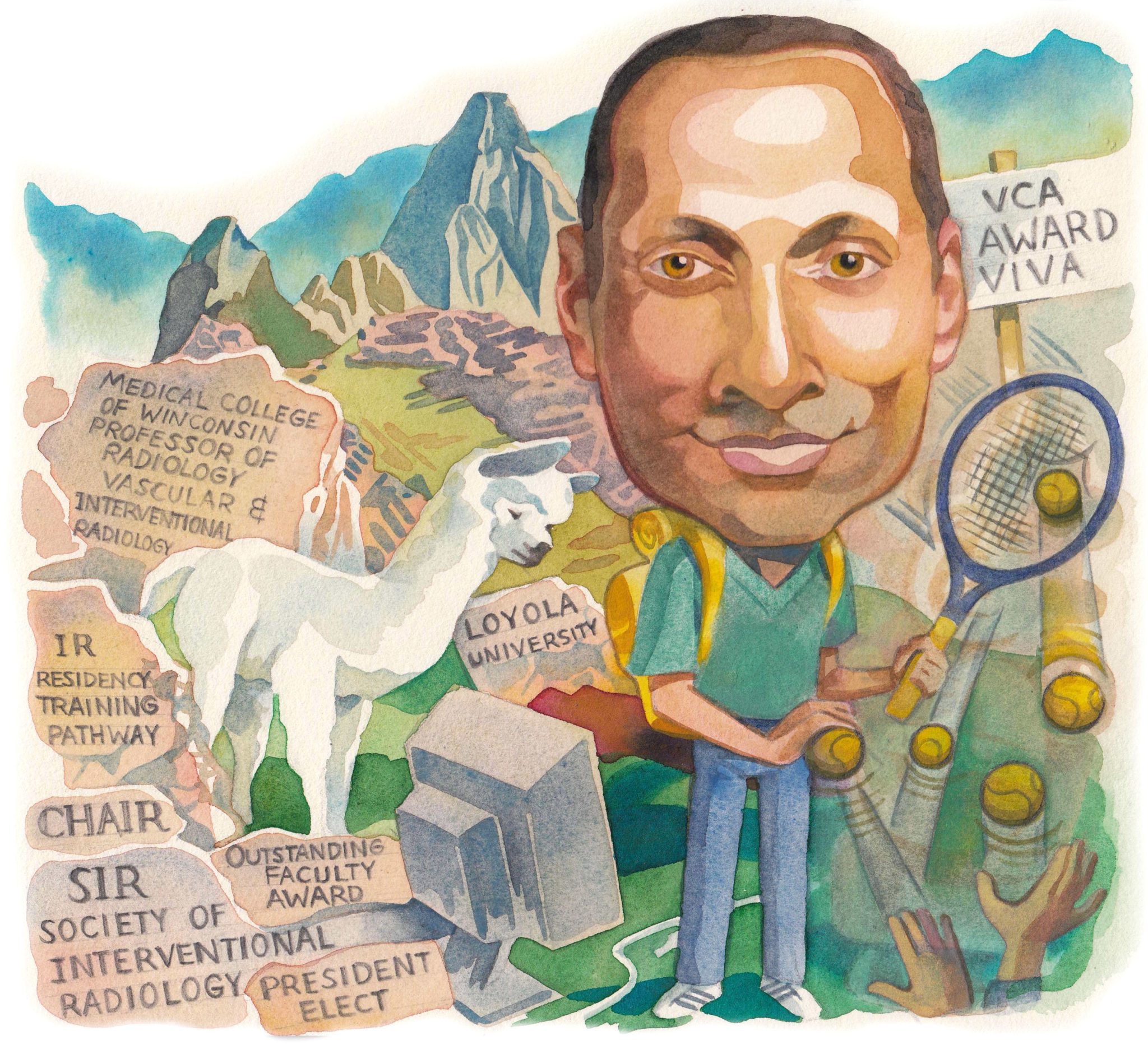
 From an early understanding in medical school that interventional radiology (IR) was “the future”, Parag Patel has dedicated his career to the discipline, notably as a primary investigator of the BEST-CLI and ATTRACT trials, and now as the incoming president-elect of the Society of Interventional Radiology (SIR). He has also been integral to the design and implementation of a universal IR education curriculum in the USA. In so doing, he has played a large part in shaping that future he once envisioned.
From an early understanding in medical school that interventional radiology (IR) was “the future”, Parag Patel has dedicated his career to the discipline, notably as a primary investigator of the BEST-CLI and ATTRACT trials, and now as the incoming president-elect of the Society of Interventional Radiology (SIR). He has also been integral to the design and implementation of a universal IR education curriculum in the USA. In so doing, he has played a large part in shaping that future he once envisioned.
What initially drew you to interventional radiology?
I entered medical school with no knowledge of the field. I loved patient care but wanted to be able to treat the pathology as well. All of my medical school research was done within vascular surgery. During my surgery clerkship, we routinely followed our patients for tests or studies. One such patient had a postoperative bleed and I assumed we would go back to the operating room, but instead we ventured down to “Special Procedures” (a thankfully historic term for interventional radiology [IR]). Marc Borge successfully embolized the bleeding source. That was my first exposure to angiography and the opportunities that it provided—I was hooked. That was such a light bulb moment for me. IR was the future. Innovative, elegant, minimally invasive, and, in my mind, the future of medicine. I was all in.
Who have been important mentors throughout your career?
My parents instilled in me a genuine work ethic as well as respect and appreciation of your fellow persons. They gave up so much certainty to provide for me and my brother as immigrants to the USA. Much of who I am today is because of them.
With regards to IR, Marc Borge introduced me to the specialty and fostered a young, naïve, but genuinely interested trainee. Nicos Labropoulos served as a research mentor and emphasised the importance of good science and knowing the data. As a resident, Marc invited me to attend the local Chicago angioclub, which at the time had many leaders in the field that impressed on me the ingenuity and novelty of the specialty. I was fortunate to train at Miami Vascular. Jim Benenati and Barry Katzen led a phenomenal group of faculty that instilled the importance of true clinical practice, exhibiting leadership and grace under pressure. I was privileged to join the group in Milwaukee and continue my growth under the leadership of Bill Rilling, Sean Tutton, Rob Hieb, Eric Hohenwalter, and soon after Sarah White, formed a small but formidable group of interventional radiologists that grew our clinical practice. We supported each other’s research, education, and clinical efforts through a model of shared leadership.
I was very fortunate to receive support from gracious mentors, and can only hope to serve a similar guiding role for other young trainees. This is much of the driving force behind my desire to continue as programme director of our vascular and interventional radiology (VIR) fellowship [that of the Society of Interventional Radiology (SIR)], and now IR residency training programmes.
You have been a primary investigator of the BEST-CLI trial since 2014. Why is this study important?
The BEST-CLI trial (Randomised, multicentre, controlled trial to compare best endovascular versus best surgical therapy in patients with critical limb ischaemia) completed enrolment over a year ago and strives to complete follow-up during the coming year. The study is important as we have very limited high-quality data on the management of critical limb ischaemia (CLI) patients, specifically comparing best surgical versus best endovascular treatments. Our multidisciplinary collaborative practice at the Medical College of Wisconsin (MCW) has routinely followed a shared model of decision making with surgical and endovascular strategies employed in our local practice. Our involvement in BEST-CLI was seen as a natural extension of our practice and may shed light on how to best treat these patients or support how we already practice. Further studies in this space are needed to allow for a more structured and uniform algorithmic approach to be taken in the care of these patients.
As an ATTRACT trial investigator, what did this experience teach you, and how has clinical practice been impacted by these findings?
I learned much from my involvement in ATTRACT (Acute venous thrombosis: thrombus removal with adjunctive catheter-directed thrombolysis), namely, the exhaustive work it takes to consistently beat the drum for screening, enrolment, and follow-up and see a trial through to completion. Much credit goes to Suresh Vedantham for his leadership and effort. We struggled with maintaining clinical equipoise in the trial. We were studying the role of an approved treatment in the hopes of identifying a benefit for our patients long term. Many felt they already knew the best course for their patients and enrolment would prevent proper treatment if they randomised to the non-intervention arm. Nonetheless, the trial did not support routine use of pharmacomechanical catheter-directed thrombolysis (PCDT) for all acute lower extremity deep venous thrombosis (DVT) for prevention of post-thrombotic syndrome (PTS). This has helped inform our practice algorithm, as we no longer offer PCDT for isolated femoropopliteal DVT or in older patients with acute iliofemoral DVT (aside from those with phlegmasia). We will treat younger patients with symptomatic acute iliofemoral or iliocaval DVT in the hopes of improving acute symptoms and minimising the severity of PTS.
As chair of the SIR Residency Essentials Advisory Committee, you have been central to the development of the new online curriculum. What was this experience like?
The Residency Essentials project came about through a strategic planning exercise for the SIR. As Graduate Medical Education Councillor during the time of our IR Residency implementation, I was tasked to champion support for the new training model. The idea of a universal IR education curriculum available for all IR trainees aimed to minimise the significant differences in training experiences across the country. While the technical experiences may vary from institution to institution, the fundamental knowledge base of disease management, role of interventional therapies, and management of these patients could be taught to all trainees nationally. The project was a massive undertaking with cross-divisional collaboration within the SIR and significant staff support. It took over three years and a number of physician volunteers to develop the extensive curriculum outline, identify and curate content (video lectures, timely reviews, and assessment questions), and then neatly package them into modules available on a new learning management system. The project launched in July 2020 to great success. The content will continually be reviewed and periodically updated. The timing of this launch was in the midst of the pandemic and coincided with distance learning mandates across the country. The new Residency Essentials fits this quite nicely as it is an online curriculum. Now that the curriculum is complete, we have the opportunity to support IR education efforts abroad.
You are stepping into the role of president-elect of the SIR. What are your ambitions for the society in the coming years?
SIR, like any big organisation, is a big ship and abrupt changes are not easily handled. I hope to make incremental improvements to the organisation to better serve our members. Namely, we will continue to grow our education and research efforts, and increase awareness of IR treatments to patients and the value of IR to health systems.
What is the greatest challenge currently facing interventional radiologists?
We continue to have much work to do in placing the treatments we provide within the algorithm of management for the diseases we treat. Early on, we struggled with maintaining a hold on our procedures, when maintaining a hold on our patients should have been the focus. If we all agree that minimally invasive, image-guided interventions are the future, then we cannot complain if others adopt this strategy as long as they do it well. I think a bigger concern is why some of our proven therapies still remain outside the standard management guidelines of basic disease entities. This requires a long view with a strategic approach and collaboration amongst our stakeholders to accomplish. I believe we can do it.
What are your hobbies and interests outside of medicine?
Art, architecture, and industrial design. I am also an avid traveller, immersing myself in new cultures and enjoy any time spent in nature. Prepandemic, I have hiked the narrows at Zion National Park, down to the Colorado River at the Grand Canyon, trekked the Inca Trail to Machu Picchu, and am now (hopefully) planning a summit of Mount Kilimanjaro for next year. Family time is a priority, and I enjoy cooking up new recipes with my wife, Mona, or rallying tennis balls on the court with my two daughters, Simrin (age 12) and Siana (age nine). interventional interventional