An exciting opportunity awaits interventional radiologists with the miniaturisation of EVAR devices. The new-generation devices have shown a trend towards being lower in profile and some are designed for an entirely percutaneous approach.
In contrast, first-generation endografts had a large profile (24–27 outside diameter), were inflexible, cumbersome to deploy, worked sub-optimally in complex anatomy and had a high incidence of procedural complications. Over time, physicians have identified that with these first generation devices, there were frequent late complications such as device migration, modular component separation, high permeability and endotension, endoleaks and loss of structural integrity.
The concerns about durability of EVAR devices are based on the fact that most published trials reported significant re-intervention rates for complications such as endoleak and kinking. This weakness in durability also has an economic consideration, as the cost of re-intervention and post-procedural surveillance means that EVAR with older technology, is less cost-effective than open surgical repair.
Another challenge associated with EVAR is that only 50% of AAA patients were candidates for EVAR because half of the patients are excluded because of unfavourable neck anatomy and iliac anatomy.
“The two areas of opportunities in EVAR applicability are the proximal neck (with respect to conformability, accommodation and seal zone) and the iliac access (where profile, trackability and kink resistance come into play),” said Zvonimir Krajcer, programme director, Peripheral Vascular Interventions, Department of Cardiology, St Luke’s Episcopal Hospital and Texas Heart Institute, Houston, USA.
He told delegates at ISET in January 2011 that on the other hand newer generation devices offer ease of use, better accuracy in deployment, wider applications for challenging anatomy, low-profile delivery systems, more opportunities for non-surgical specialists and better durability. The question remains, how will device modification contribute to improved results?
EVAR moving to PEVAR era
“Learn and embrace totally percutaneous EVAR (PEVAR) techniques, or be left out,” Krajcer said at ISET.
Krajcer explained the goals of PEVAR: to reduce mortality and morbidity, hospital stay and offer a quicker return to normal lifestyle. The percutaneous approach also offers shorter procedure times and less blood loss.
“EVAR will be more frequently done in the cath lab and interventional radiology suite, due to the cost issues of operating room time, operating room personnel, equipment, anaesthesia and anaesthesiologist,” he predicted.
Krajcer noted that technological advances in EVAR delivery systems such as a reduction in profile and simplified delivery would facilitate a totally percutaneous approach. “A totally percutaneous approach to EVAR requires suitable closure devices, appropriate endovascular delivery systems, careful patient selection, expertise in technique, and proper facilities with ready access to surgical services. There is also definitely a learning curve associated with the procedure,” he said.
Krajcer clarified that not all commercially available devices are specifically designed for, or are suitable for percutaneous use. He mentioned that Endologix’s IntuiTrak, which has a contralateral percutaneous indication with a simple deployment mechanism, is “In Europe, 15% of EVAR procedures are performed in PEVAR fashion, but in Australia, 70% of the EVAR are performed in PEVAR fashion.”
Later, at the iCON meeting in Arizona, Krajcer said, “An entirely percutaneous approach to EVAR appears safe and feasible in patients with suitable anatomy. ”
He gave the results of the first multicentre, prospective, randomised controlled trial of this approach (the PEVAR trial) which was initiated in 2010 under an investigational device exemption in the USA to determine the technical effectiveness and clinical benefit of this approach. Krajcer reported the initial PEVAR trial roll-in phase results. “Enrolment has begun across the 20 participating centres and is expected to be completed this year,” he said.
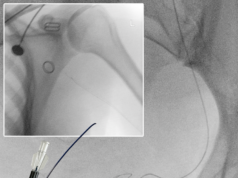
Ipsilateral ‘pre-close’ percutaneous access was performed with the Abbott Vascular’s Prostar XL or ProGlide suture-mediated closure devices.
“The PEVAR procedures were performed using Endologix’s IntuiTrak Endovascular System. Using the integrated 19F introducer sheath, the bifurcated endograft was implanted in combination with proximal or limb extensions as per the patient’s anatomy. Contralaterally, vessels were either pre-closed if a limb extension was required, or closed using standard percutaneous technique. Procedural technical success, defined as successful common femoral access and closure, was evaluated, as were vascular and systemic adverse events. Post-procedural follow-up has been scheduled at one and six months.
“Among 33 patients enrolled in the roll-in phase, technical success rates of 97% (access) and 100% (endovascular repair) have been achieved, with no major adverse events observed. Patients were discharged from the hospital at an average of 1.4 days following the procedure,” said Krajcer.
Results
A total of 24 patients (96% men), mean age of 72±6.4 years were enrolled. Mean proximal neck and aneurysm sac diameters were 27±2.9mm and 5.3±0.4cm, respectively. Patients were maintained either under general (63%) or local (37%) anaesthesia, and were treated either by vascular surgeons or interventionalists with surgeons as a multidisciplinary team. All endovascular aneurysm repairs were performed successfully. Over a mean procedure time of 117 minutes, estimated blood loss was 206mL.
In-hospital complications were limited to two blood transfusions for anaemia and one surgical repair for contralateral scrotal haematoma in a patient who underwent standard percutaneous access with manual compression for closure. Ankle-brachial indices remained unchanged from the pre-operative values to the one-month values.
Patients were discharged from the hospital at a mean of 1.4 days postoperatively. Within one month, no deaths, ruptures, conversions to open repair, secondary procedures, renal complications, or other serious vascular events were observed.