This advertorial is sponsored by Interventional Systems.

Achieving consistency, accuracy, and ease of use in interventional radiology (IR) and interventional oncology (IO) procedures, including biopsy and ablation, while limiting procedure time, can present challenges for interventional radiologists. These range from planning interventions across multiple planes without angular limitations and aligning needles to sub-millimetre accuracy, to inserting instruments securely, and all this while aiming to limit the patient and physician’s exposure to radiation.
By taking away the difficulties associated with freehand alignment and targeting, Micromate helps physicians focus on improving reproducibility, speeding up the procedure, reducing radiation dose, and deploying the system even for complex indications.

Setup
The system is table-mounted and compact, allowing close-up, full-body patient access from all angles (even inside the gantry). The robot can be mounted to any standard table, with configurable positioning arms, table adapters, and baseplates Setting up, loading DICOM data, and performing automatic registration takes less than five minutes, and when the physician walks into the room after the registration scan, the system is ready for targeting without requiring any additional steps.
Workflow integration
The clinical team need not deviate from their usual workflow, as setup is quick, the learning curve with Micromate is short—around one hour of focused, hands-on training and support on the first couple of days of cases—and there is no need for clinical support specialists to always be present in the room to use the system. Micromate also supports key imaging modalities—cone beam computed tomography (CBCT), fluoroscopy, computed tomography (CT) and CT fluoroscopy. Full ultrasound integration is under development, too.

Intraoperative planning
The system allows the physician to rely on updated intraoperative scans for planning purposes. Interventional Systems’ proprietary, intuitive software for accurately planning single or multi-needle interventions without angular limitations.
Alignment
Perform an automatic or joystick-controlled alignment with sub-millimetre accuracy to your planned trajectories within seconds with the help of navigation and live-imaging.

Instrument insertion
Micromate is compatible with all needles from 8 to 21G. The operator can securely advance their instrument of choice under live imaging while keeping haptic feedback. Lateral system deviations to the trajectory during and after instrument insertion are signaled by the system, allowing for correction.
In summary, Micromate decreases user and patient radiation thanks to its live imaging capabilities, navigated alignment, and misalignment detection, and it reduces the need for control scans.
Subscription model supplements Micromate’s procedural advantages
In addition to the advantages Micromate affords the operator in terms of consistency, accuracy, and ease of use, the system also has the benefit of being more affordable than similar robotic planning and navigation devices. This is the case thanks to a subscription option the company offers centres who wish to use Micromate for their percutaneous procedures.
Subscriptions are flexible depending on how many patients the hospital may require the system for, and there is no upfront capital investment or mandatory service agreement. The user instead pays a monthly fee that includes access to free software updates, as well as the robotic platform itself. The monthly service also includes disposable covers and needle guides and specialised onboarding assistance for the initial cases.
In conversation with Pedro Costa

Pedro Costa is the CEO of Interventional Systems and he took time to sit down and speak to Interventional News about the company’s origins, vision, product offering, and what he is most looking forward to achieving in the near future in the medical robotics and navigation space with Interventional Systems.
The conversation begins at the beginning of the company, which Costa explains was founded in 2010 by Michael Vogele. It originated from a product Vogele had developed for “patient positioning using moveable tables to get an optimised radiation therapy treatment”, which then became an exploration of whether the patient could “stay still, and you move the therapeutic instruments”—relevant for interventional and surgical procedures, Costa highlights. “And then Interventional Systems was founded.” The company today, he continues, “develops solutions for different applications, and interventional oncology [IO] is one of these”. Endo-urology, cranial neurosurgery and spinal surgery are the other areas that Interventional Systems works or has worked in, Costa informs. “Now we have grown our team and [we are continuing] to look for other surgical areas where we can make a difference—that is it in a nutshell,” he summarises.
One system offering multiple solutions
Costa then seeks to clarify a key aspect of the company’s offering—a miniature robot as opposed to larger systems that solve “the clinical accuracy problem” only. These tend to be repurposed from their original industrial applications and so only provide “incremental” advantages, whereas Interventional Systems’ focus is creating robotic devices “from scratch”, Costa qualifies. The robot—Micromate—can be used “with any image device”, and is “simple, affordable” and allows for “fast training”.
Homing in on affordability, Costa next addresses what it is about the Interventional Systems offering that ensures this for customers. Hospitals rarely get reimbursed for the use of robotic systems, he explains. Therefore the focus is on proving that the cost of investment will be offset by the advantages the robot will bring, such as procedural accuracy and reduced radiation exposure. “So, for us, it is all about the quadruple aim of providing less expensive care […] by controlling the whole supply chain so that we are still able to keep viable margins, while [offering a good price].” Costa relays how surgical robots can cost up to €1 million, but Interventional Systems’ is around €200,000 and “our price per procedure is less than €200”. He goes on to underline a key feature of the company’s offering: the subscription model. “Those hospitals that cannot buy a system upfront, they are able to subscribe and pay a monthly fee […] Patients can then be treated using the technology without the need for a huge investment by hospitals.”
Practicality is another factor that Interventional Systems has considered, Costa proceeds, in terms of greater usability for staff, but also a better patient experience. “We have been able to prove […] that with two days’ training (that include already initial cases on patients) you should be ready to fly solo.” He adds that starting with using the robot for simple cases lends itself to gradually moving on to using it for more complex cases, to the point where all cases become “routine”. Moreover, from a patient point of view, Costa adds, the patient spends less time under anaesthesia when anaesthesia is used, and less time—almost half of what it would be without the system—in the operating theatre overall. Radiation exposure can be reduced as a result by “close to half”, he celebrates. All this offsets the cost of the robot, according to Costa, “and it is better for everybody”.
Cultivating ‘centres of excellence’
Interventional Systems has a scheme whereby they partner with the hospitals that use Micromate, “rather than just [being] a supplier”. The relationship with the hospital is ongoing, Costa details, and there is a cloud-based ‘academy’ environment though which staff can access “everything from case reports to training, to narrated cases and videos from other physicians”. Users can also store information on the platform, Costa elaborates, and share tips or presentations with the rest of the user community. “Everyone can crosspollinate and learn from each other” while going through “sequential steps to learn and train with the technology”. There is also the capability of contacting the Interventional Systems team with queries, Costa supplements further. “It is a way for us to provide continuous training and value without being there and it is available 24/7.”
Beyond this, Costa goes on, is the idea of having a “symbiotic partnership” with around a dozen interventional radiology/ endo-urology departments, which will gain the title of ‘centre of excellence’ in return. “We understand that for IR and interventional oncology [IO], there is no silver bullet, you cannot say ‘this robot will solve all problems’,” Costa avers, but he emphasises the value robotics can bring, and especially in cooperation with interventional radiologists. This is because the technology is designed to solve the most pressing of the “thousands” of problems within IR, “with different organs, needles, and in different procedures”. For the ‘centres of excellence’, Costa conveys how the company absorbs a proportion of the installation costs for Micromate in return for the interventional radiologists in those centres “giving back to the community by sharing their experiences”, including study results. This will help other physicians, and also the company, in terms of shedding light on “which areas to focus on [developing] and which not” going forward.
What the future holds
Costa turns to reflect on the “year-on-year growth in terms of users” that Interventional Systems has seen, including outside Europe and the USA, which indicates “interest in the technology” and, as Costa sees it, “that robotics is here to stay”. He refers to the expansion of the navigation technology market outside robotics too, pointing out that this market competition will “enable” the continued growth of the company, to the benefit of interventional radiologists.
Micromate offers “[definite] added benefit” according to user of 13 years

Marco van Strijen is an early adopter of Micromate (Interventional Systems), having used the robotic assistance system for over a decade at St Antonius Ziekenhuis (Nieuwegein, The Netherlands). At the 2023 European Conference on Interventional Oncology (ECIO; 16–19 April, Stockholm, Sweden), Van Strijen delivered a symposium to discuss why he uses Micromate in his specialist non-vascular intervention and interventional oncology practice. Among the features that set the technology apart when it comes to planning and executing needle placement for his procedures, Van Strijen highlighted its multimodality compatibility, how it compares to freehand needle introduction, and its proven clinical performance for ablation and biopsy.
Van Strijen began his presentation by outlining the “challenges [we have] as interventional oncologists,” which include patients moving if they are not under general anaesthesia, moving anatomy as the patient breathes and their heart beats. Another challenge is when one has to resort to “steep approaches to avoid critical structures in the thoracic cavity,” Van Strijen noted, and “the difficulty of trying to enter oblique planes during bone interventions, where the needle can easily slip off the intended path”.
The advantages Micromate affords
With these obstacles to overcome, Van Strijen described the benefits robotic assistance can afford those in his line of work as it “improves the accuracy and reproducibility of every single needle intervention we perform”. He added that robotic systems such as Micromate are “also very helpful in reducing human error and the learning curve time [and…] robotics can help speed up procedures, thus potentially limiting complications”. Speeding up the procedures also involves reducing the radiation dose for the operator, according to the speaker. “We are now capable of expanding our interventions [to lesions and indications] considered too complex or too distant.”
Next, Van Strijen homed in on how Micromate lends itself well to specific types of cases. “I do a lot of lung biopsies,” he informed delegates, going on to describe how this requires him to navigate the “challenge of moving anatomy on breathing”. However, Micromate helps him overcome this issue, offering a “proper fix of the needle [independent of the patient for] a very stable and safe approach”. As a clinical example of complexity and stability, the case of using Micromate in biopsying a periorbital mass was demonstrated as “very easy to perform without damaging any of the critical structures close by”, and likewise, kidney cryoablation with “up to five needles” is “never really a problem,” Van Strijen shared. Thanks to Micromate, it is possible “to manoeuvre in between complex anatomy, and in my hospital, we have had a decrease in mortality over the past three years,” the speaker celebrated.
Micromate’s proven clinical performance
The presenter followed this up by addressing his centre’s clinical results with Micromate for biopsy in the initial computed tomography (CT)-guided environment. The study included seven biopsies (of the lung, spleen, and pelvic bone), and had a 100% diagnostic yield, meaning all biopsies were correctly sampled and histological diagnosis achieved, and there was one small bleeding complication unrelated to the robot. “On average we only used two to three scans per patient”, and Van Strijen also pointed out that the average radiation exposure per procedure was “very low”. More extensive study results were presented with the analysis of the prospective last 149 procedures performed with cone beam computed tomography (CBCT) needle guidance. These were compared to the results dating back 10 years from the same hospital and showed a significant decrease in procedure time (12:15m vs. 28:30m), reduction of radiation dose (6.73 mSv vs. 12.7 mSv) and an increase in diagnostic yield (96% vs. 91.4%). These results were consistent even in more complex procedures. Van Strijen also noted that comparable results were found in ablation procedures with Micromate, pointing to the fact that “as complexity increases, Micromate’s performance stays high”. Micromate allows for a lower radiation exposure, faster procedures, and equivalent or better diagnostic yields. Procedure time is 50% less than freehand and radiation exposure is not linked to how complex a case is but instead, individual patient anatomy or requirements of the case.
Regarding the complication analysis for biopsy, “the complication rate was in line with the literature despite an increase in average case complexity”. Of the 144 cases analysed, there were 13 pneumothoraces, Van Strijen highlighted, only three of which required chest tube drainage. Most of the complications occurred in lung cases—there were two soft tissue bleeds which could be treated locally, the speaker continued. The bone cases saw no complications, he added, and none of the total complications were linked to the use of the robot.
One system for multiple modalities
Van Strijen has used Micromate for CT and CBCT, and informed his audience that the main differences between CT and CBCT lie in the fact that after acquisition and planning, the C-arm angulation with CBCT is automated, whereas the gross positioning is manual for CT. Moreover, in the CBCT environment, needle placement uses fluoroscopy, whereas it is fully automatic for CT, involving no further radiation.
In conclusion, Van Strijen stated that they “definitely see added benefit [using Micromate including] in challenging cases, such as endoleak, trigeminal ablation, complex drainages, and bone interventions”. Additional benefits of using Micromate, Van Strijen reiterated, are its short learning curve, the device’s stability and accuracy, the shorter procedure time, and the reduction in radiation exposure that it affords. Finally, it is a multimodality solution, compatible with CT, CBCT, and fluoroscopy.
“This robot has helped us expand our limits”

Dimitrios Filippiadis is associate professor of diagnostic and interventional radiology (IR) at the National and Kapodistrian University of Athens (Athens, Greece), whose practice centres around musculoskeletal (MSK) interventions and diagnostics, and interventional oncology (IO) and cancer pain management. He has been using the Micromate robotic navigation system (Interventional Systems) in the computed tomography (CT) suite since November 2022, and predominantly for biopsies, neurolyses, and ablation procedures.
What benefits come with utilising navigation and robotics in IR procedures? How do you envision the future of these technologies?
Navigation and robotics can be utilised to increase excellence and “repeatability” in performing percutaneous or vascular procedures. For example, in ablation, technologies can significantly impact ablation standardisation for the better, providing invaluable services to simulation, performance, and verification of success. The greatest advantage of utilising such systems is the potential to reduce duration and ionising radiation exposure during the procedure and, at the same time, increase the accuracy of a specific therapeutic approach. However, navigation systems and robotics for IR procedures are not a panacea, are not a solution or remedy for all difficulties and they should not substitute clinical judgement. They should be used as tools for providing a patient with a better and more reliable clinical care. I hope and feel that soon, these systems will be invaluable tools assisting all operators in implementing his or her clinical thought and judgement in practice. For this to happen, a complete system giving answers to all practical steps of a procedure is necessary.
What will the role of robotics be in medical students’ education and in training new doctors?

While the utilisation of robotics is rapidly growing in everyday clinical practice, it is a fact that medical students and residents still have limited experience and familiarity with them. As robotic procedures are becoming more widespread, early exposure to their applications for medical students and residents could be an integral part of training, helping them to have more meaningful observation experience and allowing them to recognise the significance of utilising such technologies in everyday clinical practice. However, before anything else, to enhance engagement of medical students and residents with robotics, inclusion of their application in the current curricula is a prerequisite. Once this is achieved, educators will be able to consider hands-on and other simulation programmes for medical students and residents aiming to shift training in robotics to earlier during IR and other specialty/subspecialty training.
Can you discuss the current limitations or challenges associated with gaining funding for robotic/navigation technologies? How does their cost impact accessibility and widespread adoption?
It goes without saying that the current limitation of these systems is the challenge of acquiring one of them due to funding limitations, thus hindering widespread adoption and utilisation. Vendors could start reaching out to users with more flexible and less rigid financial proposals before the discussion for reimbursing navigation systems and robotics in IR procedures has properly begins. Finally, there is a need for developing a system which will contribute ease of use, reliability and repeatability in all the steps of a procedure starting from simulation to performance (through navigation) and verification of success.
What procedures have you performed with Micromate? Any interesting cases you would like to share?
The greatest advantage of Micromate is that it can be used for all kinds of percutaneous procedures. After the initial learning curve, which I have to say is quite short, mainly because the robot is extremely user-friendly and easy to master, we started using it for all the cases during which multiple apparatuses or inclined approaches are necessary. I would not want to focus on a specific interesting case. I would rather say that the utilisation of this robot has helped us expand our limits and treat lesions in extremely challenging locations during a technically easier, shorter, and more cost-efficient session.
“This crucial [planning] step of the ablation is simplified”

Alexander Kupferthaler is an interventional radiologist at the Ordensklinikum Linz (Linz, Austria) whose work is predominantly interventional oncology (IO)-based. He carried out the first computed tomography (CT)-guided liver ablation with Micromate (Interventional Systems), and beyond this, has used the system for a range of biopsies and kidney cryoablation. Kupferthaler has also used Micromate with cone beam (CB) CT and talks through his experience.
I understand you have experience using Micromate for microwave ablation of the liver. How long have you been doing this procedure? Do you use Micromate for any other procedures?
As I work in an cancer centre hospital, IO has played a major role since I started interventional radiology (IR). So, for as long as I can remember, I have done microwave ablation procedures.
I started using ultrasound guidance when placing the probes, then for the more complicated ablations, I used the previous model of the Micromate robot with CBCT guidance and image-fusion when needed. When Interventional Systems showcased their new Micromate CT-guided workflow I was quite fascinated.
I have used the Micromate system for complicated lung biopsies, bone and soft-tissue biopsies, coeliac trunk blockades, osteoid-osteoma radiofrequency ablations, and kidney cryoablations.
How does doing microwave liver ablation differ with CT vs. CBCT guidance? How does Micromate help with the challenges that each of these means of carrying out ablations present?
The major difference between the two modalities is the image quality. CT scanners typically offer higher spatial resolution, larger coverage of the imaged volume, while reducing noise and image artifacts. This offers better visualisation of the tumour, nearby blood vessels, and critical structures, while reducing the risk of complications and providing a faster workflow. And while I do prefer the Micromate CT-based navigation workflow, time for interventional procedures in the CT suite is restricted. So, whenever safe and feasible for the patient, I also use the Micromate robot in the interventional suite.
For the Micromate CT-guided workflow, Interventional Systems has developed a complete solution that assists especially in angled trajectories and complicated-to-reach lesions. Doing out-of-plane trajectories in CT is challenging. With the easy-to-use user interface of the Micromate system, this crucial step of the ablation procedure is simplified. When the planning is done, positioning the robot and placing the needles or probes is quick and straightforward.
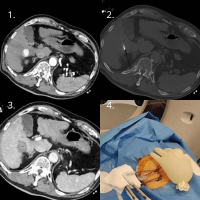
1. In liver segments V&VI there is a hypervascular lesion 2.7cm in size. Note the fiducials of the robot on the right side of the patient. 2. Out-of-plane trajectory of the microwave antenna. Contour of the robot on the top right side. 3. Final ablation zone in contrast-enhanced CT after the intervention. 4. Micromate setup for the liver ablation case.
What is the significance of the Interventional Systems armrest when doing liver ablations?
Patient positioning is the key to success in liver ablations. Most of the time, the patient is lying in a supine position on the CT table. If the arm is then positioned next to the body in an adducted position, the treatment area is limited. Thus, placing the arm on the armrest will increase the treatment area. Additionally, the armrest provides stability, prevents unwanted movement and reduces strain on the patient’s arm and shoulder muscles.
Would you be able to share some images from a liver ablation case you found particularly memorable?
I can, actually. See the images here and their descriptions, as well as a photo of the Micromate setup.









