Sebastian Mafeld, interventional radiology Fellow at NHS and co-founder of UK Endovascular Trainees (UKETS) tells Interventional News about how a three-dimensional (3D) printed model of an aorta is a valuable training tool for endovascular interventions and how printing unique catheter shapes and patient-specific devices might be around the corner.
What is 3D printing and how does it work?
Three-dimensional (3D) printing is a manufacturing process whereby an object is created by sequentially printing it in layers. A 3D printer is guided by a computer file, typically in STL (surface tessellation language) format. This manufacturing process is also referred to as “additive manufacturing”. There are several additive manufacturing technologies but one of the most common ones is Stereolithography; this works by sequentially solidifying a light-sensitive liquid compound (photopolymer) layer by layer.
One of the reasons why this manufacturing process is important is that traditionally manufacturing processes have been ‘subtractive’ (in its simplest form, imagine wood carving; pieces are removed from a block of wood until finally the model is created). 3D printing, on the other hand, is additive, this means incredibly complex designs can be created which were not possible previously with traditional manufacturing methods.
3D printing is suddenly becoming accessible. Why?
3D printing has been around for decades but has only expanded rapidly over the past few years. Peter Diamandis gives a great explanation in his book Bold on why this may have occurred. He states: “an exponential technology does not really become disruptive until a powerful, user-friendly interface exists”. While 3D printers have been around for decades, user-friendly software for designing 3D printable models has not. Now that this software is available to virtually to anyone with a computer and combined with easier access to 3D printers (just google “3D printing + your city) these factors play an important role in the evolution of this technology.

Can you comment on the key findings from your study presented at CIRSE 2016. What did the feedback from physicians who used the 3D printed vascular model suggest?
We 3D printed a scale model of the entire aorta along with its major branches in a transparent material for the purposes of endovascular simulation training. This project was undertaken together with Materialise, a 3D printing company based in Leuven, Belgium. A 6F sheath was inserted into a predesigned hole in each common femoral artery and the model was filled with regular tap water. This allowed the use of normal catheters/wires/balloons inside the model. We thought this may give a user a better understanding of how common endovascular tools behave whilst experiencing enhanced haptics including pushability, torquability, and trackability.Ninety-six physicians in training trialled the model under the supervision of an experienced interventional radiologist. Common endovascular tasks eg accessing the visceral vessels were performed. Candidates then rated their agreement with 12 statements regarding their training experience on a standard five-point Likert scale. The data from this was presented at CIRSE 2016 in Barcelona, Spain. Our data shows a trend towards “strong agreement” that this 3D printed model was a valuable learning tool for training in basic endovascular skills. Candidates also generally agreed that catheterisation of vessels and manipulation of the guidewire was “realistic” inside the model.
Where does 3D printing fit into the healthcare setting?
Despite a lot of excitement about 3D printing in healthcare, its exact role in healthcare has yet to be established. There are countless reports for unique uses of 3D printing, most of which centre around printing structures for improved anatomical understanding. Other areas include the printing of implants for craniofacial/skeletal surgery. As medicine is shifting towards a “personalised” instead of population-based approach, 3D printing reflects this theme by allowing patient specific products to be created.
How can 3D printing impact procedure planning/ simulation? Are there any data to suggest improved treatment outcomes from using 3D printing technology?
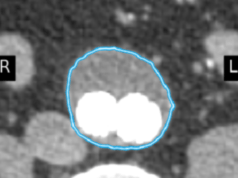
From an endovascular standpoint, 3D printing may be useful in procedural planning and device testing. For example, in the treatment of complex aneurysms, 3D printing can allow visualisation of an aneurysm and evaluation of stent graft suitability. The ability to physically test critical parts of an endovascular procedure using a 3D printed model might lead to reductions in procedure time and radiation exposure or improvements in outcomes and patient safety. However, at present, I am not aware of any large scale published data which demonstrates improved treatment outcomes from using 3D printing in endovascular practice or any other field of medicine. Biglino et al have published some data showing that the 3D printing of patient-specific models of congenital heart defects can improve communication between cardiologists and parents. It is imperative that data is obtained to establish the potential impact 3D printing can have on procedures in all areas of medicine.

Specifically, what endovascular applications are there for 3D printing?
In terms of implantable 3D printed devices, endovascular practice lags behind its orthopaedic and maxillofacial counterparts. While there have been many reported cases of 3D printed bone implants, I am not aware of any 3D printed implanted endovascular devices. Currently, the endovascular applications for 3D printed have mainly been focussed on creating models for procedural planning and device testing. In is possible that patients have benefitted from 3D printed vascular models as companies and physicians have been able to better test their devices prior to deployment.
What are the challenges for 3D printing in the healthcare setting?
3D printing faces the same challenges as many technologies in medicine; regulation, time, technical skill, cost, and validation.
As 3D printing in medicine is a rapidly evolving field but currently lacks large-scale evidence, regulation is challenging. The FDA, however, has released draft guidance in 2016 entitled “Technical considerations for additive manufactured devices” – which marks a step towards regulating this area.
Being able to accurately 3D print a medical model from imaging data requires detailed anatomic understanding and the ability to use software. If we are going to base treatment decisions on 3D printed models then we need to be confident about the software and printer’s ability to accurately reproduce the anatomy in question. Patient safety is always paramount, therefore robust validation systems are needed to ensure accuracy.
The speed of 3D printing is also highly variable, small models can be produced relatively quickly while, for example, our model took 96 hours to print as it was made up of over 5000 layers. The time taken to produce the STL file necessary for 3D printing must also be considered in an era where healthcare professionals are increasingly overstretched.
Anecdotal evidence from case reports or small series may support the value 3D printing, but is not enough to understand whether it will remain a novelty or become a necessity. Large scale data are necessary to determine the impact of 3D printing on medical procedures, and to establish a cost:benefit analysis.

What does the future of 3D printing in endovascular practice look like?
In the short term, I think we will start to see more patient-specific devices being produced. For example, in challenging anatomies we might be able to print unique catheter shapes to facilitate procedures. In the longer term, the 3D printing of endovascular stent grafts or other implantable devices may be possible. If we look even further to the hypothetical future, rather than departments keeping large stocks of multiple device sizes, companies might instead provide a 3D printer which can produce a patient-specific device on-demand. 3D bioprinting of blood vessels is also an evolving area which may have unique endovascular applications. Overall, I remain optimistic about the technology’s future in endovascular practice.