The role of interventional radiology in the management of severely traumatised patients began three to four decades ago with the embolization of the internal iliac arteries for massive pelvic bleeding. Over time, interventional radiology has progressively taken on a principal role in management of trauma patients.
Trauma is the leading cause of death in people younger than 45 years of age, and the main cause of death in children. There are three main type of trauma: blunt trauma as caused by car accidents, assaults, blows, falls from heights etc; penetrating trauma, as caused by bullets, stab wounds, impalements; and iatrogenic traumas caused or generated by physicians and healthcare workers. This latter category is not reported, recorded or registered adequately.
The trauma team includes trauma surgeons, other surgeons, radiologists, interventional radiologists, anaesthetists, ancillary personnel, etc.
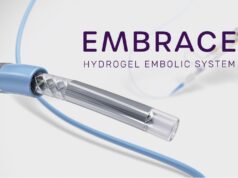
The main interventional radiology methods for trauma care are: embolization with temporary or permanent particles and agents such as coils, plugs, and even glues; stenting with different kinds of stents and/or stent-grafts and placement of balloon occlusion catheters in injuries to large vessels such as the aorta or inferior vena cava.
Severely traumatised patients must be brought to a trauma level one facility for care. The concept of bringing patients to the nearest facility is obsolete and associated with a high mortality. On the other hand, speed is also of essence and the “first hour” is critical in trauma care. Trauma patients lose blood and become hypotensive, hypothermic, coagulopathic, hypoxic, and acidotic unless the bleeding stops or is stopped by surgeons or interventional radiologists, or both. Interventional radiology should be involved in the care of the trauma victims, even before they arrive into the emergency room.
Multiple detector CT scanning plays a primordial role in the evaluation of trauma patients. Most emergency rooms use CT scanning for “triage” of trauma patients. Unstable patients go to the operating room for surgical control. Stable patients go to interventional radiology for control or to the intensive care unit for non-operative, conservative management.
The hybrid suite, the room of the future for trauma care, now exists all over the world. It consists of a sterile operating room with state-of-the-art angiographic imaging. There are facilities for anaesthesia and other imaging such as intravascular ultrasound, ultrasound and Dyna CT. All interventional radiology and surgical procedures can be carried out in the suite. Patients arrive to the emergency room and directly to the hybrid suite, then get full body CT scan within the next 90 seconds. With all the team at the side, a decision as to management is then made on the spot. A collaborative, rather than a competitive approach, with all healthcare workers involved in trauma patients, is strongly encouraged.
Surgical and interventional radiology intervention
Severely traumatised patients who are actively bleeding and haemodynamically unstable, must go to the operating room directly as there is no time for diagnostic imaging. Laparotomy can be done to stop or temporise bleeding. Thereafter, the patients can be brought to the interventional radiology suite for definitive management. Interventional radiology management of injuries is potentially easier, cost-effective, safer, and may prevent altogether or make smaller, limited surgery. The patients can go home earlier, and back to their work too. As such, it is our opinion that interventional radiology alternatives in treating trauma patients must be emphasised during medical school training, and thereafter.
Pelvic trauma
Patients with pelvic trauma usually die from bleeding and its complications. Therefore, the IR management is ideal. As soon as pelvic bleeding is suspected, the patients are evaluated by CT scanning. If the CT shows active bleeding, the patients undergo arteriography, and embolization of both internal iliac arteries, even if only one side is bleeding. Embolization is done with temporary particles (those that recanalise in days or weeks), or permanent ones that do not recanalise at all. These traumatised patients are usually young and have abundant collateral supply, therefore, bleeding may continue from collaterals, if only one side is embolized. Moreover, the risk of ischaemia to pelvic organs is low or absent for the same reason: collateral supply. Mortality rates from pelvic bleeding have significantly decreased since 1976 when interventional radiology management by pelvic arterial embolization has been utilised.
Chest trauma
Severe blunt trauma to chest, such as in a car accidents with decceleration mechanisms, may result in injuries to the heart, and is usually lethal. Acute traumatic rupture of the thoracic aorta results in death at the scene 80–90% of the time. Those who survive and arrive in the emergency room are immediately studied by CT. If thoracic aortic rupture is found, it can be fixed with stent grafting. The time of the intervention is controversial, but recent evidence indicates that it is no longer necessary to repair it as soon as the diagnosis is made. At this time, we prefer to wait until the patient is in a better condition to tolerate repair in an urgent rather than emergent situation.
Abdominal trauma
Is common and secondary to car accidents and/or gunshot wounds. Haemodynamically unstable patients go immediately to the operating room for temporary stopping or controlling bleeding from solid organs such as the spleen and liver, and this is very difficult to do with open surgery. Thereafter, the patients return to interventional radiology. Renal injuries are managed surgically by partial or total nephrectomy. On the other hand interventional radiology preserves the kidneys and bleeding is easily controlled with embolization. Surgery is needed to fix injuries and perforations of hollow viscerae. Solid organ injuries are easily and readily managed by selective embolization. Splenic salvage is a good thing in children and young adults. A major operation is avoided or made smaller, and faster recuperation is expected. Biliary injuries are managed with percutaneous techniques. Large vessel injuries are extremely serious. Stent grafting of traumatic abdominal aortic rupture or inferior vena cava, although rare, is readily done by interventional radiology. Bleeding from the aorta or inferior vena cava is lethal, but placement of occlusion balloon catheters is a life-saver.
Peripheral trauma
Interventional radiologists are the principal operators to fix traumatic injuries to blood vessels of the extremities: arteries usually, and veins on occasion. Bleeding sites can be readily embolized with particles or coils. Perforations, pseudoaneurysms and arteriovenous fistulae can be managed with with stents of different types and configurations: covered or uncovered, self-expanding or balloon-expandable. Interventional radiology management rapidly restores limb circulation and ischaemia is avoided, resulting in a major reduction in amputation rates. At this time, the management of traumatic vascular limb injuries has improved considerably due to dramatic improvements in endovascular techniques.
Central nervous system trauma
Head trauma is usually managed by our neurosurgical and interventional neuroradiology colleagues. Interventional radiology occasionally carries out embolization of severely damaged vertebral arteries. Significant bullet injuries to brachiocephalic vessels are easily managed using stents by the “peripheral” interventional radiology or by the neuro team. Internal carotid artery stenting is done in sporadic instances. Carotid blow out syndrome is a catastrophic entity associated with significant mortality and morbidity, and is successfully managed by stenting and/or embolization of the internal and external carotid arteries. Bleeding sites in the face, neck or brain from bullets, knives and/or car accidents are embolized with relative ease.
Jaime Tisnado is professor of Radiology and Surgery, VCU Health System, VCU Virginia Commonwealth University, Richmond, USA. He has reported no disclosures pertinent to this article.