Early data from the prospective multicentre AVeVA study that employed a covered stent (Covera; Bard, now BD) to treat stenoses at the venous anastomosis of arteriovenous graft access circuits has shown superior results when measured against predicted benchmark data.
Bart Dolmatch (Palo Alto Medical Foundation, Palo Alto, USA), speaking on behalf of the AVeVA investigators at the Leipzig Interventional Course (LINC; 30 January–2 February 2018, Leipzig, Germany) presented the six-month data from the study that is ongoing to two years.
“It is was widely known that arteriovenous grafts have a high rate of stenosis at the graft-to-vein anastomosis and that post-angioplasty recurrence of this stenosis is common. Most arteriovenous graft failures, whether it is poor flow, ineffective dialysis or thrombosis are related to this stenosis,” Dolmatch explained.
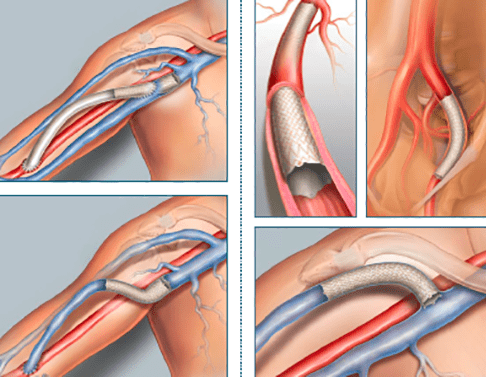
The Covera Vascular covered stent comes in two configurations, either flared or straight to accommodate for diameter differences in arteriovenous access anatomy, and is an ePTFE covered, helical, nitinol stent that is available in various sizes.
The AVeVA study is a prospective multicentre, non-randomised study with 110 patients who were enrolled and treated at 14 investigative centres in the USA. “The objective was to treat stenotic lesions at the graft-vein anastomosis of arteriovenous grafts with the Covera vascular covered stent and assess safety and patency,” said Dolmatch.
There was a clinical events committee that adjudicated safety events. The endpoints were measured against performance goals since there was no comparator control group.
Demographics and lesion characteristics
Data reported at LINC revealed that there were 110 patients of whom just over half were female. Most lesions treated were restenosis lesions. “Most stenoses are treated with balloon dilation and then recur, and these constituted nearly 72% in the study,” noted Dolmatch. The mean lesion length was 24.1±15.5mm; the mean baseline target lesion stenosis was 75.1%±14.8%; and a quarter of the patients had thrombus either at the time of presentation, or within 30 days of presentation.
Endpoints
The primary endpoint was safety through 30 days freedom from protocol (defined as safety events in the arteriovenous access circuit, not including stenosis or thrombosis) with a performance goal of 88% derived from the literature.
Target lesion primary patency (TLPP) at six months was defined as the time from the study procedure until the next clinically-driven reintervention at the treatment site, thrombotic occlusion, surgery, or permanent access abandonment. The control was a performance goal of 40% derived from the literature and pivotal studies.
Secondary endpoints include technical and procedural success; access circuit primary patency (ACPP; the time until the next access thrombosis or clinically-driven repeated interventional anywhere in the access circuit); index of patency function (the time to study completion or access abandonment divided by the number of reinterventions to maintain vascular access).
The upper arm was the access site in the majority of cases (98%) and therefore, the flared configuration of the stent was most commonly used. There was almost no residual stenosis after the procedure, noted Dolmatch.
“A first look at the AVeVA data shows that there was 94.6% freedom from a primary safety event at 30 days, which was superior to the performance goal of 88% (p=0.002).The 70.3% TLPP rate at six months, which was the primary efficacy endpoint, was superior to the performance goal of 40% (p<0.0001). With regard to secondary outcomes through six months, there was a 100% acute technical and procedural success rate and 39.2% six-month ACPP rates. The target lesion intervention rate was 0.41 at six-months and access circuit intervention rate is 1.05 the same follow-up point. The follow up in the AVeVA trials is ongoing through two years,” said Dolmatch.










