
The US Food and Drug Administration (FDA) convened today and yesterday for a General Issues Panel Meeting on the late mortality safety signal associated with paclitaxel-coated products (i.e. paclitaxel-coated balloons and paclitaxel-eluting stents) used to treat peripheral arterial disease (PAD) in the femoropopliteal arteries.
Following the two-day discussion, an FDA Circulatory System Devices Panel Advisory Committee concluded that there is a “mortality signal” as first described in the Journal of the American Heart Association (JAHA) paper authored by Konstantinos Katsanos et al (Patras, Greece) in December 2018, but that better data collection was necessary going forward, as some data were missing. The panel determined that there were not enough data to confirm a class effect, and no consensus was reached on the cause(s) of death.
“One of the take-aways from this has been that in this field of lower extremity revascularisation, the quality of these data and the rigour of these clinical trials has been somewhat amiss, that even with the adjustments in follow-up, anywhere from 6% to 26% of the patients’ data are missing at one and five-year follow-up,” surmised Todd Rasmussen, a vascular surgeon in Kansas, USA.
On the second day, themes of the meeting included the risk-benefit consideration for patients, and how best to convey the choice of paclitaxel treatment in the context of short-term benefit and improved quality of life weighed against a signal of late mortality risk. The panel largely agreed that patient choice is central, as clinical benefits are clearly demonstrated and increased quality-of-life may be an acceptable tradeoff for long-term risks for many patients.
Furthermore, consistently noted throughout panel discussion was the importance of collaboration between industry, regulatory bodies and other stakeholders to ensure data gaps are filled and strategically tackled. Recommendations regarding future study designs as well as optimisation of ongoing trials were discussed, with no consensus on the value of registry data as opposed to more time-consuming and expensive randomised controlled trials. However, FDA representative Bram Zuckerman stated in the last hour of the meeting, “Unfortunately, we have a signal here that remains undetermined. One of the reasons why is that the death adjudication uniformly in these FDA trials was poor.” He summarised, “going forward, mortality will be given a higher priority, and we will need to think about how it can be best assessed and adjudicated.”
The panel agreed that in terms of determining efficacy, studies can follow up to one year for these endpoints, while safety should be assessed over a longer-term follow-up of three to five years.
Concluding the meeting, Bram Zuckerberg states that the two-day meeting and presentation has been “extremely helpful” for the FDA, who will now consider the analysis of the panel, and “look forward to continued collaboration in this field.”
See below for highlights from 19-20 June:
As laid out in an Executive Summary document prior to the meeting, the aims of this meeting are several-fold. They are to review the available information and provide feedback on:
- The presence and magnitude of a late mortality safety signal;
- Whether all paclitaxel-coated vascular products (regardless of device platform or dose) are associated with the signal;
- The impact of missing data and covariates on the signal;
- Potential mechanism of death (causality) considering drug dose exposure and pre-clinical data;
- Reconsideration of the benefit-risk profile related to the use of these products;
- The need for the collection of additional data and/or device labelling changes;
- The impact of the signal on ongoing femoropopliteal disease clinical trials as well as on paclitaxel-coated products marketed or under clinical evaluation for other indications (e.g. treatment of stenoses in arteriovenous dialysis fistulae, critical limb ischemia).
To date, FDA analyses of available data from FDA-approved devices show an increase in late mortality between two and five years associated with paclitaxel-coated devices intended to treat femoropopliteal disease. However, the FDA note in their Executive Summary report, “causality for the late mortality rate increase could not be determined”. The agency recommends that additional data are needed to further assess the magnitude of the late mortality signal, determine any potential causes, identify patient sub-groups that may be at greater risk, and to update benefit-risk considerations of this device class.
Live updates on the meeting below:
19 June, 13:00 BST
Chairing the panel, Richard Lange opens the meeting, and a statement from Evella Washington of the FDA outlines the selection for the panel members, who have been chosen as financially impartial with no conflicts of interest.
19 June, 13:15 BST
Eleni Whatley gives the first presentation to introduce the background and the purpose of the panel. Day one will focus on the presence and magnitude of the mortality signal described by Katsanos et al, whether a class effect is identified, and potential causal mechanisms. On day two, Whatley states, dose effect will be considered along with the benefit/risk profile of paclitaxel devices and finally a discussion of future regulatory actions, including modifications to clinical trial designs, approved product labelling, and additional studies.
Whatley summarises the recently completed analysis by the FDA and outlines the Executive Summary, which is available here: https://www.fda.gov/media/127698/download
19 June, 13:40 BST
Mathematical statistician Adrijo Chakraborty notes “the FDA statistical team conducted a sensitivity analysis to evaluate potential impact of missing data on mortality analysis.”
The findings of this analysis were summarised by Chakraborty as follows: “The meta-analysis results suggest that there is an increasing risk for mortality in patients treated with paclitaxel-coated devices compared to control devices for the as treated population. Similar chain is observed for the intent-to-treat population. The meta-analysis here are based on a small number of studies, based on four studies and analysis of four year and five year are based on three studies. The FDA conducted a sensitivity analysis to evaluate the impact of missing data. The results suggest that the increases risk of mortality remains for the scenarios completed. It is to be noted that the result is the choice of the data.”
Yu Zhao, a second mathematical statistician, reports the FDA conducted a gender analysis to assess heterogeneity and treatment effect regarding cause to mortality between male and female in a similar fashion as the geography analysis. “For all four pivotal RCTs, no evidence of differential treatment effect between the paclitaxel-coated device group and the uncoated device group was no difference between the gender groups,” Zhao says.
19 June, 13:50 BST
Donna Buckley, Interventional Radiologist, presents the FDA’s cause of death analysis, and says “The mortality rate for each cardiovascular subtype was numerically higher for the paclitaxel group versus the non-paclitaxel device group in all subcategories.” Overall, “there were no qualitative trends identified to suggest a particular cancer type was more frequent in the paclitaxel group”, and other causes of death investigated included adverse events classified into 27 FDA specified categories.
“The results qualitatively suggest a higher percentage of patients treated with paclitaxel-coated device groups had more adverse events in all categories except injury”, Buckley says. “Overall, patients treated with paclitaxel-coated devices had higher rates of all death types versus patients treated with uncoated devices, except for infection related deaths and trauma, which trended higher in the control group. There’s also no clear trend from the data provided that treatment with paclitaxel-coated devices was associated with excess rate of cardiovascular or non-cardiovascular death subtypes.”
In terms of causal mechanisms, Buckley notes: “There was no specific group of adverse events identified that would suggest a mechanism for late term mortality and a baseline characteristics and was not specifically instructive, and more detailed statistical analysis would need to be conducted to identify potential covariates and predictors of mortality.”
Summarising the full FDA analysis, Buckley states: “With regard to subgroup analyses, there was no consistent pattern of differences in gender and geography across the studies to suggest a predictable differential treatment effect between patients treated in the USA and outside the USA in male and female patients. With regard to the adjudication of causes of death and adverse events, there were numerous limitations such that conclusion should be viewed with caution. However, given the data provided, FDA were not able to determine a pattern in cause of death or adverse events that would indicate a clear area of exploration regarding a potential biological mechanism.”
19 June, 14:15 BST
Buckley adds, in discussion with the panel, that “one of the challenges that we have for most of the studies there were some restrictions at least in terms of use of paclitaxel-coated device and ipsilateral land within the first 12 months. Beyond that it became a little bit more challenging to collect that data in a robust way.”
Panel member Frank W LoGerfo questions the follow-up on death in non-US studies, where social security numbers may not be implemented, and whether there may be more missing data in non-US trials.
Panel member Joaquin Siguroa states: “a challenge of potential identification of cause versus confounding variables present in risk factors as they evolve in an underlying disease state which has with it associated high mortality and morbidity, in a disease state in which we know effective therapies for secondary prevention are often not prescribed or not compliant. And so trying to identify where that signal comes from remains a challenge which we’ll continue to explore.”
Considering the significant amount of comorbidities in this patient population, Buckley says the cause of death was often unclear, especially at five year follow-up. “I’m not tremendously confident, I think the industry did their due diligence in trying their best to adjudicate those events, but given the patient population I think it was extremely challenging to end up with a very confident single cause of death in those cases,” she says.
Whatley expands on this point, noting that “these randomised controlled studies were not designed to look at five year mortality.”
19 June, 14:45 BST
Combined industry presentations begin.
Daniel Clair, advisor to Medtornic and Boston Scientific and a consultant for BD, provides a pan-industry talk on the “dramatic” and “critical” role drug-eluting technologies have played in patient care. “We believe this technology is safe, effective, and incredibly valuable for our patients and the healthcare system overall”, he says. “To address the issues or the concern regarding paclitaxel and mortality, industry competitors have become partners in an unparalleled way to provide additional information and analysis regarding each of their studies. Honestly I have not ever witnessed this type of collaborative effort on the part of companies living in a very competitive environment to assess the safety and performance of an entire class of devices. Their interaction and cooperation exemplify for clinicians the commitment to ensure the therapies they are offering enhance the options for patients without putting them at increased risk. I am proud ton stand with them as a partner in this effort.”
“Paclitaxel has a long history of use in the vascular system”, Clair reminds the audience, calling the value of paclitaxel devices “indispensable” in the coronary arteries. He says their use in this space informed the later decision to use the drug in peripheral vessels.
Describing the industry response to the FDA letter of 15 March earlier this year, recommending paclitaxel use being limited to patients at greater risk of restenosis, Clair says: “While the intent of this letter was patient safety, the impact of the communication is significant. For many clinicians, health care systems have unilaterally made the decision to withdraw these devices from their shelves. And for many physicians the fear of potential lawsuits has led to these products being essentially unusable in the current environment. For our patients, this means a dramatically increased risk for intervention failure and risks related to reintervention, potentially limb loss in more severe cases. For some patients, this will mean only surgical options will be offered or no treatment at all. And I would particularly like to emphasise the potential impact for our most vulnerable patients, those with critical limb ischemia. These sickest and most frail patients with PAD may be subjected to increasing numbers of interventions, and they have the highest riskof restenosis along with the potential to be pushing to more extensive therapies, which increases their overall mortality and local risk of the rocedures. These patients need these devices.”
“There is no relationship between paclitaxel dose and mortality”, Clair says. He reiterates: “There is no evidence of paclitaxel-related toxicities in the mortalities.”
19 June, 15:00 BST
Aaron Lottes, lead scientist for Zilver PTX (Cook Medical), promises to provide clinical data confirming no mortality signal seen with paclitaxel across the company’s 25 year history with the drug.
As other paclitaxel devices were not available at the time, Lottes says that the original Zilver PTX RCT and Japan PMS provide the best data available to look at paclitaxel data. These compared the Zilver PTX to a bare metal stent (BMS).
Patients enrolled in the Zilver PTX RCT were randomised to percutaneous transluminal angioplasty (PTA) and Zilver PTX. Any cross-over (patients who moved from the PTA to the Zilver PTX group) were analysed as belonging to the paclitaxel group. Forty per cent of the patients initially randomised to PTA were actually analysed as Zilver PTX patients after crossing over.
Michael Dake now provides updates on the clinical results of this study.
An intent to treat analysis is “generally recognised” as the standard for evaluating effectiveness. However, Dake says, “To address questions of safety, regulatory guidance, literature and expert opinions agree that we must consider how patients were actually treated.” As 40% of patients enrolled in the BMS arm of the Zilver PTX RCT were treated with Zilver PTX, he says an intent to treat analysis “is not an appropriate method for answering the question of paclitaxel mortality.”
He says the Katsanos et al data did not account for this crossover, but when Cook Medical accounted for it in their own analysis,”Mortality rates for Zilver PTX and PTA bare metal stent groups were comparable. FDA’s analysis confirms that there was no mortality signal for Zilver PTX”.
In addition to treatment with paclitaxel, the Cook Medical investigators looked at the dose effect. They report finding no association of dose with mortality.
Concluding, Dake says: “We are here because of statistical debate that has raised questions with patient safety. Paclitaxel devices with proven benefit are being restricted from use and these decisions are negatively impacting patient care. Analysing Zilver PTX patients in the PTA stent group does not make sense. When Zilver PTX patients are analysed base on how they were actually treated, the published results for the overall meta-analysis of paclitaxel related mortality become non-significant. That is, there is no class effect. If Zilver PTX patients are analysed based on how they were actually treated, the results for the entire published meta-analysis of paclitaxel-related mortality become non-significant. An appropriate assess must be based on actual treatment with paclitaxel not on how patients were randomised. When appropriately analysed the data clearly shows no mortality signal with paclitaxel stents.”
19 June, 15:15 BST
JD Meler speaks on behalf of BD. He provides an overview of three randomised controlled trials involving the company’s Lutonix drug-coated balloon.
Vascular surgeon Kenneth Ouriel now speaks on behalf of BD. Outlining the Bradford Hill criteria, designed to tease out a difference between association and causality. Ouriel says there is no evidence for causation between paclitaxel and mortality, echoing Dake’s earlier remarks (see above).
“If causation does exist, there should be one or more specific causes of deaths more prevalent in the DCB arm, causes corresponding uniquely to the mechanism of action”, he says.
He continues: “An independent medical advisory committee made up of intervention lists and oncologists reviewed narratives and source documents for the 173 deaths in the Levant 1 and Levant 2 datasets. No deaths were classified as related to paclitaxel based upon the known side effects of the drug.
“Since this might not capture paclitaxel-relatedness from unknown mechanisms, we reviewed causes of death at categorised by the committee. Mechanistically, if paclitaxel caused deaths, there should be a disproportionate frequency in one category or in a group of related categories, a disproportionality that was not observed. Without clustering of death within a category, causation is not supported.”
Questioning if there was an association between dose of paclitaxel and mortality, further analysis of the Levant 2 dataset demonstrates no dose response, according to Ouriel.
“We also looked at the effect of subsequent interventions with paclitaxel devices which increased drug exposure”, he says. “Some of the analysis that had been reported to date did not account for reinterventions. Almost 20% of subjects in the Levant 2 RCT were treated with a paclitaxel device at some point during their five year follow up. And subjects in both arms, PTA and DCB, who subsequently underwent intervention with a paclitaxel device had a higher five year survival rate than those that did not. This finding was confirmed in our other studies. These findings are counterintuitive if additional paclitaxel exposure is harmful in the long run. It should be noted that the mortality rate in Levant 2 study was lower than the pad population as reported in the Swedish vascular registry at five years.”
Concluding the talk, Meler returns to the stage. He states: “There are no statistically significant increases in hazard ratio for mortality in any Lutonix study. When the Levant studies are pooled the hazard ratio is nearly one. There is no plausible mechanism for mortality or evidence of paclitaxel causation identified. And there is no increase in mortality with additional exposure to paclitaxel in either cohort. Reducing interventions is advantageous to patients, but it also reduces additional visits with health care providers, and associated benefits which may ultimately impact mortality. This creates a plausible explanation for the numerical difference.
“Finally, based on all the analyses to date and a large dataset, Lutonix DCB continues to offer meaningful benefit relative to risk in indicated patients. BD is committed to ensuring patient safety and minimising risk and we will continue to monitor safety data on Lutonix DCB in our ongoing clinical programme and in commercial use. BD plans to incorporate additional analyses into our labeling in coordination with the agency to inform physicians and patients of all available information.
“We have a large dataset that has enabled us to rule out causation. However, analysis of even larger datasets that are appropriately structured to evaluate overall patient health may be required to enable additional investigation on the subject of association.”
19 June, 15:30 BST
Following an introduction by Simona Zannetti, Peter Schneider presents data on the IN.PACT IDE and IN.PACT Japan on behalf of Medtronic.
Stressing the benefits of these devices, Schneider says: “Evidence strongly supports the benefits of DCBs. They are a major improvement from what we had to offer our patients previously, and as a result, DCBs have been integrated as standard of care into clinical practice. IN.PACT DCB has demonstrated durable effectiveness in a population of patients and this is sustained through five years. In my opinion, if we restrict the availability of paclitaxel DCBs, we would be turning back the clock to an era of less effective treatments and will likely result in more repeat interventions over the long-term.”
Laura Mauri provides a safety analysis of the Medtronic data. Pooling data from the IN.PACT Admiral IDE and the IN.PACT Japan study, Mauri says, reveals no statistical difference in the incidence of mortality between the PTA arm and DCB arm.
The pooled analysis from Medtronic also reports no gradient of risk (of mortality) according to paclitaxel dose. “Dose was not significant when examined in multiple ways”, she says.
Mauri concludes that the IN.PACT Admiral DCB is safe and effective, but adds that Medtornic “recognise that even these pooled randomised trials are underpowered to detect a difference in mortality.” She calls for “real world comparative studies followed for a sufficient duration of time” to help to better understand the long term safety of paclitaxel products.
19 June, 15:45 BST
Jonathan Batiller, head of Medical and Clinical Affairs at Philips, introduces the company’s presentations on Stellarex data. “We recognise the importance of the work that was published by JAHA in December of 2018″, Batiller says, adding “we realise there are recent publications that arrive at a different conclusion.”
William Gray explains, “After the publication of the JAHA paper, Philips prepared a prespecified analysis of mortality using the data collected from controlled trials using the Stellarex DCB.” In an integrated analysis of all seven Stellarex studies, Gray says the findings “continues to support a low all-cause mortality through 3 years of 7.9%, and compares favourably to the 9.3% pooled randomised Stellarex DCB mortality rate.”
“There is no mortality signal of it with Stellarex we could not find in all of our analysis,” Gray concludes. “We’ve reliably shown this through sizable randomised analysis through single trials through DCB and these are consistent observations. The lack of mortality signal further reinforced the paclitaxel cross-over accounting. Comparing paclitaxel exposure versus non paclitaxel exposure further supports paclitaxel as not contributing to mortality, and absent a complete accounting of paclitaxel exposure in any analysis, and its potential impact on modified as treated outcomes any large scale assessment will be incomplete. And we continue to believe that the benefits of Stellarex outweighs its risks, and improved patients out comes in the long term.”
19 June, 16:00 BST
Ian Meredith, executive vice president and global chief medical officer at Boston Scientific, says their Eluvia drug-eluting stent is “differentiated from other paclitaxel coated technologies used in peripheral vascular disease: Its stable polymer does not break down as compared to all DCB excipients that do break down and contribute to downstream particulates.”
Meredith presents data on paclitaxel use in the coronaries. “Paclitaxel in the treatment of peripheral vascular disease and coronary vas clear disease is safe and effective”, he states. “The design principles of Eluvia and coronary stents are identical in coronary studies to studies comparing paclitaxel stents with bare metal stents, and any effect of paclitaxel would have been observed in those taxus studies.”
Robert Lookstein presents further data on Eluvia, including an ongoing large randomised controlled trial. With “extremely high clinical follow-up” at two years (n=398) all-cause mortality is 6.5%, which is “not distinguishable from” the mortality rate reported in the FDA panel pack. Lookstein reports “to date, we’ve seen no mortality signal whatsoever for the Eluvia drug-eluting stent.”
“The clinical benefit observed with the Eluvia drug eluting stent is observed in all patients studied to date,” Lookstein states, and points out, “The paclitaxel eluting coronary stents, the taxus extent and drug-eluting stent were not included in the JAHA meta-analysis we’re not included in the long term outcomes for the FDA panel pack and were not included in the subsequent VIVA Summit.”
19 June, 16:15 BST
In a final discussion and Q&A before the lunch break, panel member John Hirshfield says “we are being subjected to a forest of duelling numbers: Body counts, crude mortality and subjects under observation, but also all derived coefficients that are derived from these numbers. The problem is that the numbers presented by industry and the numbers presented by the FDA are not the same.” Hirshfield expresses his hope from the panel, to “get a real common agreement of what the actual numbers are between the sponsors and the agencies so we know exactly what data we’re dealing with.”
Panel member David Kandzari adds to Hirshfield’s point, noting “I’m not sure if it’s just the numbers issue or not, I’m trying to sort out two very disparate groups of presentations this morning”.
Panel member Bram Zuckerman says that while the FDA data has been verified, Zuckerman cautions: “I would be careful about utilising of the most up-to-date data analyses. They have not been checked by the FDA, and I can say in general terms, because of a multitude of problems, the FDA has had a lot of back and forth with each company to verify data.” Nevertheless, Zuckerman acknowledges the industry has “stepped up to the plate” in what he calls a “dynamic process”.
19 June, 17:30 BST
Andrew Holden takes to the podium to detail the results of his latest paper, published earlier this week in the Journal of Endovascular Therapy (JEVT), which report finding no causal link between paclitaxel dose and all-cause mortality.
He says: “Probably the biggest limitation in the [dose] equation is the fact that the authors had to use lesion length because they only had summary level data to assist. But of course, lesion length is a poor representative of dose delivered because we do not know the number of balloons used, the amount of overlap, and even treatment beyond the target lesion.”
19 June, 19:30 BST
Presenting the questions for the FDA, Eleni Whatley first permits the panel to discuss the potential presence and magnitude of a late mortality signal associated with paclitaxel devices.
With the panel in agreement in terms of the presence of a signal, the panellists each expressed their concern. Whilst Katsanos’ data was held in high regard, the effect of missing data was discussed at depth, eliciting a variety of responses from the panellists.
“One of the take-aways from this has been that in this field of lower extremity revascularisation, the quality of these data and the rigor of these clinical trials has been somewhat amiss, that even with the adjustments in follow-up, anywhere from 6% to 26% of the patients’ data are missing at one and five-year follow-up,” surmised Todd Rasmussen.
The second question pertains to class effect. “Discuss the strength of the evidence supporting late mortality risk class effect among all US-approved devices,” inquires Whatley, urging the panel to answer irrespective of platform, dose or formulation. The panel expressed a clear consensus that there are not sufficient data to “definitely rule in or out a class effect.”
Although Bram Zuckerman (FDA) alludes to the idea of a new trial comprising a large number of patients, he questioned the panel on whether they are okay with the poolability of devices to address such needs.
Thirdly, the panel are questioned on the impact of missing data, a notably reoccurring topic of today’s meeting. Again, the panel highlight the impact of incomplete data, which, they say, may make the overall data look better or worse if it were to be reported; in turn affecting efficacy analyses.
Moreover, Zuckerman emphasises that increasing the quality and follow-up will not stop after the current evaluation. “This is a very disappointing experience for all. This problem now has significant ramifications,” he adds, and he stresses the need to improve evaluation moving forward.
The penultimate question put to the panel concerns the added value of subgroup analyses. “No clear trends were observed based on region or gender. In addition, baseline characteristics were compared between patients that died and patients remaining alive at the end of available follow-up period for the pivotal studies. In general, patients who died were older with more comorbidities and had longer lesion lengths compared to surviving subjects. However, no consistent pattern was determined,” summarised Whatley.
Addressing the panel, she asks them to discuss the issue of whether such analyses help identify specific patient subgroups that are at increased (or reduced) risk of late mortality following treatment with paclitaxel-coated devices.
However, the panellists maintain that no particular subgroup signal that identifies who might benefit or, more importantly, who might be at risk from drug devices. The consensus calls for more data, and specifically, more heterogeneity within it.
The conclusive question concerns the cause of death. “Do the cause of death data support the presence of a late mortality signal associated with paclitaxel-coated device treatment and suggest a mechanism for this signal?”
Evoking a variety of responses, the panel ultimately concedes that they do not feel comfortable with these data concerning the correct attribution of death. Thus, the panellists also express a lack of consensus regarding whether the data conveys a clear mechanism for such a signal.
20 June, 12:00 BST
The panellists resume their positions, with chairman Richard Lange opening the second day of the meeting. “For today’s agenda the panel will discuss and make recommendations on recent observations of increased long-term mortality and peripheral arterial disease patients treated with Paclitaxel compared to uncoated comparative devices. The FDA requests panel input regarding the presence and magnitude of the signal and potential causes. The FDA also seeks input regarding appropriate regulatory actions associated with the findings.”
Introducing the FDA’s presentation today, Eleni Whatley (Lead Reviewer) acknowledges that given the new information regarding long-term clinical mortality, the FDA reevaluated the preclinical animal studies that were conducted on the five approved devices. She concludes, “Regardless of low dose and single administration, paclitaxel was resident in local and downstream tissue for 60 days and beyond, and in some cases for as long as 270 days. Through no relationship could be gleaned from paclitaxel concentration and local tissue effects, there is the potential that the drug could be having an effect on various tissue systems during its residence and thus allowing for chronic effects.”
Karen Manhart provides an overview of an analyses of the preclinical safety study data. Summarising the studies on animal safety studies, she says, “[There were] no systemic pathologic changes which appear to be device or drug-related. The reviewed data does not suggest a potential mechanism for increased late mortality observed in human study subjects.” Yet she adds that it is important to understand that chronic time-points for animal study data is still short-term compared to the observed safety signal.
Next, Donna Buckley (Interventional Radiologist) presents the dose analysis conclusions. “ZILVER PTX TCT, IN.PACT SFA I and II displayed no clear relationship between dose and mortality. LEVANT 2 RCT shows a possible trend of increased mortality with increased dose.” However, she points to the fact that no consistent association between dose and mortality was detected across studies.
Weighing up the benefits versus the risks of TLR, Buckley surmised, “Overall the class of devices that includes use of Paclitaxel coating to inhibit restenosis have shown consistent and generally sustained benefit in the reduction of reintervention to treat femoral popliteal disease. It is important to emphasise that a qualitative comparison of these findings should be cautioned given that TLR and mortality events are not comparable given differences in severity. Also these events do not fully characterise the totality of the device benefits and risks.”
In relation to the next steps of PAS and labelling, Buckley posits, “Overall, based on the review of the available data, there appears to be a trend of increased mortality three to five years following treatment with Paclitaxel coated stents or balloons in the femoral popliteal arteries. However, as previously emphasised, there are numerous limitations with the currently available clinical data and the result and analysis. In addition, a biological or non-biological cause responsible for this late mortality signal is not evident.”
She adds: “Regarding a new RCT, a fundamental question for the panel is whether a randomised trial of Paclitaxel coated versus uncoated devices is feasible.”
Considering the specifics of labelling, she notes, “[Given] the FDA’s least burdensome principles approach, it may not be possible at the time of device approval to fully predict long-term safety and effectiveness. Note that FDA required for all Paclitaxel coated devices that the pivotal study subjects be followed up to five years as part of the condition of PMA approval, following the collection of these post approval data—whether related to the post approval studies in place or related to new agreed upon data collection efforts. In addition to updating the clinical data, other appropriate modifications may be made to labelling in order to convey appropriate safety information.”
Finally, Buckley concluded the FDA’s presentations for the day: “The FDA reevaluated previously conducted animal PK and safety studies and did not identify information that may suggest a potential mechanism for late mortality. We investigated the observed Paclitaxel doses in the pivotal trials, and did not identify a relationship between mortality and Paclitaxel dose that was consistent across all trials. We also investigated clinically driven TLR in pivotal studies and for all time points the risk ratio values favoured the Paclitaxel device group at five years. The FDA identified approximately 20% decreased risk of clinically driven TLR with patients treated with Paclitaxel coated devices benefit in this regard. This should be considered when we discuss risk and overall adjustments for the risk profile of these devices.” She urges the panel to provide discussion and input on these topics.
20 June, 14:15 BST
Combined manufacturer presentation begins.
Laura Mauri, vice president of global clinical research and analytics at Medtronic, opens the discussion, introducing her fellow speakers Daniel Clair (University of South Carolina, USA) and Eric Secemsky (Harvard Medical School, USA).
Clair gives an anecdote from the recent National Vascular Meeting, where an informal poll revealed that many attendees no longer used paclitaxel devices, demonstrating how the Katsanos et al paper has had “a significant impact on physicians’ ability or hesitation to use these devices”. Clair says it will be good to get closure and clarity on this topic, therefore.
Looking at the use of paclitaxel devices in specific vascular beds, Clair reports no difference in mortality in patients treated with paclitaxel devices compared to without. This held true in the coronary arteries, in arterio-venous access usage, in renal arteries and in below-the-knee patients, Clair informs the audience.
Laura Mauri takes to the podium. She reiterates that the trials discussed yesterday were focused on a narrow patient population and “do not reflect the full spectrum of patients that clinicians see”. She also makes the point that the RCTs under scrutiny were not powered to analyse mortality.
“Real-world analyses, when done properly, can be helpful, but they are not good at avoiding selective bias. They are much more precise, but it is not more convincing to have more precise but biased estimate”, she says. “The only time we can rely on real-world data is if there are robust methods that we are confident about to adjust for selection bias”.
“The study designs were not designed for long term mortality. Regarding paclitaxel treatment; one important thing to point out that has not been stressed before is that we also do not know the treatments that were received before randomisation in almost all of the studies. Drug treated products were available to patients before they were entered [into randomisation], many patients had prior procedures and were being treated for a second time and that was not recorded whether they had had paclitaxel before randomisation”, Mauri criticises.
She summarises: “The observational studies in this space have to be evaluated very carefully and we have to look at those that have been conducted with a high attention to methods. They increase the precision and, if they are reliable in terms of the methods, can be quite important. It is important to know there are unique strengths for this observational data; one is that the completeness and mortality data may actually be better than the randomised trials, which is shocking but true. […] The take home message is in these conducted studies is there are a large number of patients studied representing non-overlapping groups of patients, and hazard ratios are really all right around one with very tight confidence intervals.”
Secemsky says that having a comorbid disease could “negate or impact the potential harm of drug-coated therapy”. He explains: “One of the strengths of our Medicare analysis is the size – not that we have 150,000 patients, but that when we do look at separate subgroups, we have enough patient population to find a meaningful follow-up. I want to highlight here that 60% of our patients are non-CLI patients. In the PAD world, there are two groups of patients, high risk and low risk. High risk are CLI and the non-risk are claudicants and non-CLI. Here we have 90,000 patients; we have more than 17,000 patients contributing data through 1,250 days, we find that there is no associated risk or evidence of harm with drug coated therapy with an upper limit of our confidence interval at 0.96.”
Laura Mauri summarises the industry response to the FDA panel questions. See image below.

“For the ongoing studies, it is important that we educate our sites about the importance of good follow-up, and then think about methods in the consent to provide for complete vital status ascertainment with linkage. We can ensure that there is better recording of additional information post procedure, as well as pre-procedure, and maintain that throughout the follow up, not just at the time of randomisation, as well as the important factors of medical therapy that are now incompletely ascertained”, Mauri recommends.
“We would like to work with the FDA to update our datasets and analyses and reflect that in the labelling, and maintain the current indications,” Mauri says.
Outlining her further recommendations, Mauri says that “It is critical really that we continue to assure patient access to treatment. These are very effective products, and we believe that the totality of evidence is supportive in terms of the benefits and risks of these devices. And right now health care providers are not fully able to do what they think is appropriate for their patients.
“We respectfully request the FDA update the 15 March letter to health care providers, really to convey the totality of evidence that is being discussed now”, Mauri says on behalf of Medtronic and industry more generally.
20 June, 14:50 BST
In the discussion following the industry presentations, temporary member Karla Ballman (Weill Cornell Medical College, New York, USA) says that she is “a bit hesitant”. She expands: “I just want to make the observation that I think we need better clinical trial design. When there is an issue with randomised data, you cannot rescue it with very large observational datasets. We take a huge step back if all of a sudden we say we do not even need to do clinical trials, we just neat the observational datasets – we could extend this [discussion] to that extreme. Why do any clinical trials in the first place? So I think there is a place for observational studies, I think they are good for hypothesis-generating, but they are not good for confirming efficacy or clinical benefit. This is why we have clinical trials. Even if they [observational studies] are done well, you can minimise some biases that are in there, but you cannot eliminate them.”
There are general calls from the floor for more information on intervention-free survival rates, which are not known.
20 June, 15:15 BST
Open public hearing session 2 begins.
Evalina Washington, the designated Federal Officer, reminds speakers to provide disclosures at the start of their talk. The FDA has received 14 requests to speak.
The first speaker is Lindsay Machan, an interventional radiologist from Vancouver, Canada. He is one of three that patented the use of paclitaxel for vascular disease, and starts by saying he believes in the drug’s safety and efficacy in treating these patients. Describing early research on the drug, Machan describes how, contrary to research presented by Whitely yesterday, his team “found that paclitaxel is an exquisitely potent inhibitor of angiogenesis at nanomolar concentrations. In fact”, he continues, “even lower than that it was the strongest angiogenesis inhibitor that we identified. In fact, we found paclitaxel did not have any endothelial cell toxicity until we got to 50 micromole concentrations, at least three orders of magnitude greater than we even could detect smooths muscle cell apoptosis.”
“The other thing we found is that the biological effect is extremely localised,” he says. “I work with a group of scientists who have among us greater than 100 man years of experience investigating the local application of paclitaxel and none of us can conceive of a mechanism for this nonspecific mortality.”
20 June, 15:25 BST
Renu Virmani, cardiovascular pathologist and president of the CVPath Institute, says: “CVpath has performed preclinical studies in drug-coated balloons for Lutonix, Medtronic, Spectranetics and now Boston Scientific; we have the largest registry for coronary stent including arteries and have published more than 200 publications regarding stents. I have examined over 100 autopsies of individuals receiving coronary paclitaxel-eluting stents – the cause of death was in no way related to paclitaxel.”
As was also presented this morning, Virmani tells attendees that preclinical studies in swine do not support toxic effects of paclitaxel with the use of DCBs and DESs for the treatment of PAD. Virmani concludes that the major cause of mortality in PAD patients is underlying CAD. “I suggest unrestricted use of DCBs and DESs, monitor and perform autopsy studies, moving forward to be certain of the cause of death”, she advises.
20 June, 15:32 BST
Erica Mayer, a breast cancer pathologist from Boston, USA, takes to the podium. She reviews data from cancer patients demonstrating the benefits of adjuvant paclitaxel.
In a trial of 6,000 patients randomised to anthracycline-based chemotherapy or paclitaxel, Mayer says that “The addition of paclitaxel reduced the risk of recurrence”, and that this what led to approval in 1999 of the drug. She adds that long term follow up showed “there was a decreased risk of all cause mortality at seven years in patients who received paclitaxel, so receiving paclitaxel helped to save lives here. There was also no increase in cardiovascular toxicity or secondary malignancies in patients who received paclitaxel.”
She also says she uses paclitaxel in pregnant patients: “We have seen no increase in maternal or fetal mortality with exposure to paclitaxel, so we feel comfortable enough with this agent that we can give it to pregnant patients.”
She concludes that paclitaxel is established as a safe and effective chemotherapy drug, and that she knows of no data reporting long-term mortality associated with paclitaxel in the oncologic space.
20 June, 15:39 BST
Ramon Varcoe, a vascular surgeon from New South Wales, Australia, speaks of trial design.
“How can we determine whether the finding of this [Katsanos et al] meta-analysis were due to paclitaxel or due to bias from clinical trial design?” he asked. Speaking of his team, he says “We had this idea to perform an identical meta-analysis of randomised controlled trials in the SFA but to exclude all drug-coated devices, so we took paclitaxel completely out of the equation. Our systematic review identified 22 studies that fulfilled the inclusion criteria. […[ Our risk ratio was highly significant at 12 months, showing the patients in the control arm had around 69% fewer mortality compared to the experimental arm. We thought this was quite compelling.”
He concludes: “What we have demonstrated here is that randomised control trials which compare types of experimental controlled trials of SFA can find additional risk of death at 12 months. We see the same risk at 24 and 30 months although we are underpowered and not significant. What if they were independent of paclitaxel completely? In my mind that casts considerable doubt as to the causal link between paclitaxel and mortality.”
He recommends “a more tenacious follow up protocol of those subjects in the experimental arms combined with higher rates of medical interaction in those RCT arms that have more frequent TLRs”.
20 June, 15:46 BST
Alik Farber (Boston, USA) speaks about the BEST-CLI registry. He comments: “The BEST CLI trial and opinion registry will provide a comprehensive and granular dataset on a sizable cohort of patients with CLI treated with paclitaxel devices. So we will be able to provide the use of paclitaxel and its procedure by calendar year by specific arterial segments throughout the course of the study, including reinterventions. We are going to be able to comment on all cause mortality and specific causes of death.”
20 June, 15:51 BST
Yann Goueffic, PI of the BATTLE trial, provides insights from this dataset. The trial compares the Zilver PTX DES with a bare metal stent with a primary endpoint of freedom from in-stent restenosis at one year. Updating the Katsanos meta-analysis with the two year data from the BATTLE trial, “we have no more signal of death in the DES group at two years”, he says. In the BATTLE trial, “there is a trend to have more deaths in the BMS group rather than the paclitaxel-eluting stent [arm]”, he informs listeners. However, he also notes that the BATTLE trial was not powered to assess safety, and so says that “no conclusions can be drawn from this secondary end point.”
20 June, 15:57 BST
Kim Hodgson, representing the Society for Vascular Surgery (SVS) as its president and chair of its paclitaxel safety taskforce, outlines the society’s vision for a pathway forward. He says: “Based on the Katsanos and other subsequent analyses, we assumed a mortality signal would be confirmed. We also assumed this panel would be hearing a lot about patient safety. Striking the right balance requires weighing the increased risk associated with extra interventions against the presumed increased mortality of paclitaxel.”
He says the SVS recommend a spectrum of actions. One is to limit paclitaxel use in claudicants to the anatomic lesion criteria of their original approvals. The SVS should work with RAPID, a public-private partnership, going forward, he says.
20 June, 16:04 BST
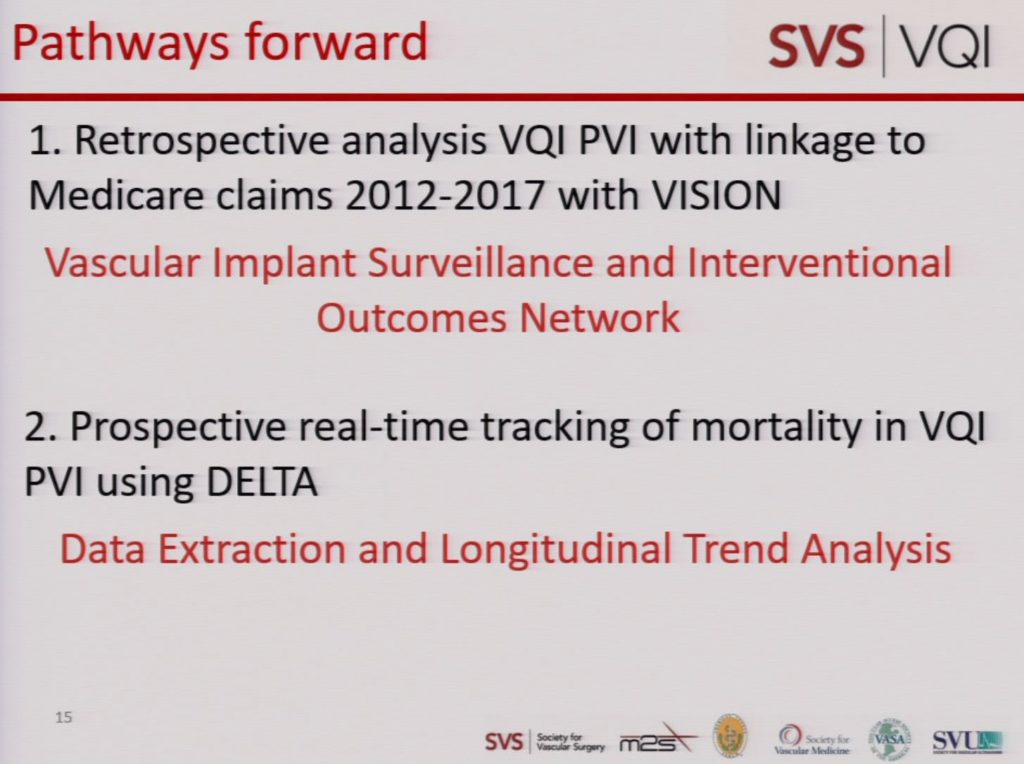
Daniel Burgess presents the SVS-VQI registry data. He says he sees two pathways forward, see below:
20 June, 16:10 BST
Schuyler Jones, a cardiologist, speaks now. He believes “There is the opportunity to do traditional observational analyses with adjustment for patient and procedural characteristics that have been described already.” He says “I think our huge challenge and with that the opportunity, is to do prospective registry-based randomised control studies with not just our registry but multiple registries for all of our patients who are cared for in the vascular space.”
His slide on possible next steps:

20 June, 16:17 BST
Statistician Rose Ann White provides her insights. She warns that “We need to be aware of the assumptions.” She adds: “I think we do change over time due to learning [referring to clinicians], and so does our practice. And we can be most efficient through cooperation.”
20 June, 16:23 BST
Stephanie Fox-Rawlings of the US National Center for Health Research praises the FDA’s continued post-market surveillance: “while there are still many questions, the fact that this [mortality] signal was seen in a solid meta-analysis is important. It is a reminder of the value of long-term studies conducted after products are on the market. It also shows the importance of FDA’s continued role in post-market surveillance and communicating about their findings to physicians and patients. This information is absolutely vital for health care providers and patients to make informed decisions about their care.”
20 June, 16:25 BST
“What is unique about my opinion today”, says John Winscott, a cardiologist from Jackson, Mississippi, “is my volume. If you look at the number of patients I have treated with drug-coated balloons in the last four years, I have treated almost 2,400 patients with drug-coated balloons, which is more patients than the [Katsanos et al] meta-analysis and randomised trials all combined.” He gives examples of positive patient stories, playing recording of patient’s testimonies to the beneficial impact paclitaxel therapy has has on their quality of life.
“I would say I have an extremely busy practice and I fight for limb salvage every day. The most powerful tools I have been able to put in my toolbox over the years has been drug-coated balloons, and the biggest change in my practice I have seen in 11 years has been drug-eluting technology. With over 2,000 patients treated and with lesion lengths around 25 centimetres, I personally do not have any concerns for safety or increased mortality. I can tell you honestly that if my mother needed a procedure tomorrow in her femoralpopliteal segment, I would not only request, I would demand she be treated with this technology”, he states.
20 June, 16:31 BST
Robert Yeh of the Beth Israel Deaconess Medical Center (Boston, USA) speaks. Detailing a study of 20,536 patients treated for PAD in the femoropopliteal arteries, he reports no statistically difference in all-cause mortality between patients treated with and without paclitaxel devices. He concludes: “In our interpretation in this large national cohort of PAD procedures, drug-coated devices were not associated with a difference in mortality. These real-world cohorts are more representative of patients undergoing treatment in routine practice, and these conclusions of device safety are more relevant to public health than those seen in the trials.”
Clarifying this statement in later questioning, Yeh says: “I think my main point is that the patients that we see in these observational datasets are actually the ones that are representative of the patients that we are treating in practice. And the one that have public health problems.” He does not believe real-world datasets should replace RCTs.
20 June, 17:40 BST
Eleni Whatley responds to questions in the final FDA Q&A session with industry.
Ian Meredith picks up some unanswered questions regarding the Boston Scientific data, clarifying dose and mortality at 5 years, saying “There is no all-cause mortality difference between bare metal stents and the paclitaxel drug-eluting stent in double blind trials. These are double blind trials with up to 100% follow-up, and the main trial driving this has a 95% follow-up.”
Laura Mauri, representing Medtronic, tells the FDA panel in response to prior questions: “In our trial we had 85% relative risk reduction, so as you expect you see a hazard ratio of 0.13, for the use of the DCB versus PTA which is highly significant; p-value less than 0.001, so that’s the first thing: the treatment is effective. And that’s true after adjusting for the one factor that was an additional independent predictor, prior peripheral revascularization, which is an independent predictor of TLR as we would expect clinically.”
Richard Lange, points out the FDA panel is tasked with “doing a couple things”: one is the address the issue of ascertainment bias, and secondly to pursue comparative analysis of US- versus non-US populations. In response, JD Mueller representing BD, says: “We were able to pull data from our resilient trial and we thought it was relevant because it compares a bare metal stent to PTA and femoral popliteal, and you can see not significant numerical difference of difference in mortality with BMS and PTA with BMS being slightly higher, so we wanted to give you an example of a non-drug related study where we also saw this ascertainment bias as an example.”
Following responses from all industry presenters, Richard Lange notes, “So what I’m seeing is in all the companies is an improved follow up, there was still a change, it was just not quite as big.”
Speaking to the point of US- versus non-US populations, Yu Zhao points to data for several trials: ZILVER PTX, LEVANT and IN.PACT data all showed the trend of a “generally sicker” population in the USA, Zhao says.
Responding to a question from LoGerfo on how bias in the timing of TLR is avoided, and why patency was not used instead, Dan Claire says: “These trials are designed to try and be set up to evaluate the effect on patients. Stenosis has an effect on us as clinicians, TLR has an effect on patients in terms of what they’re subjected to.” He continues, “I agree with you, it might be much easier to standardize how you evaluate stenosis with duplex criteria, but it’s a lot easier to get a sense of what the impact on a patient is by looking at TLR.”
Peter Schneider and William Gray both present comments on the Medtronic and Philips data, respectively, to show that quality of life “improves significantly with fewer reinterventions” using DCBs.
Panel member Gary Jarvis summarises the day’s work, saying “We know what we know now, we know what we don’t know and don’t have, and we’re going to discuss here in a minute where we’re going to go”. He adds that following the publication in JAHA last year, “everybody has been talking about this”, and cooperation between industry, societies and regulatory panels has been significant. “And that is one thing I hope that industry does, is to continue this collaboration beyond this meeting”, Jarvis says.
Panel member Patricia Daigle, representing consumers, says “as I consumer, my concern is the consumer choices. I think the consumer has the right to be aware of the risk-benefit, but ultimately the choice should be up to the consumer. […] The consumer has a right to have a qualitative and quantitative life, and it’s their choice to decide which type of life they would like to live.”
20 June, 18:30 BST
The potential relationship between paclitaxel dose and mortality is assessed by the panel largely as “inconclusive”, as the data is limited and “unclear”, and insufficient to establish any dose-response relationship. Krucoff notes that “the other important thing from my point of view is that this is not a dose assigned, this is a dose-driven largely by anatomy, by lesion length, etc. So I think the dose-response relationship here is fundamentally confounded, in the data—and the data available don’t make it simple.”
Summarising the thoughts of the panel, Lange says: “it is inconclusive based upon the data, it’s complicated by patient variables including length of lesion, and there’s a concern about high tissue levels intraarterial and intraluminar as well.”
20 June, 18:40 BST
Discussing preclinical models, Krucoff says “in this type of safety signal exploration that anything and everything we can learn from preclinical models we should maximize our efforts to adding knowledge rather than having to explore human risk to change ignorance into knowledge.”
Bram Zuckerman underlines Krucoff’s point, adding human trials are both time consuming and expensive. However, Joaquin Cigarroa argues that while he “wholeheartedly agrees” with the statements of Krucoff and Zuckerman, “as designed, the current approach to preclinical animal studies will be unable to adequately address the question of is this signal associated with a biological plausible model.”
Do you feel additional preclinical studies would be helpful? While a majority on the panel voted yes, Todd Rasmussen says “this would be going backwards. […] I don’t think there’s no use to animal studies, I’m not trying to be argumentative, but I just offer the balance that, when we have something that is acknowledged now as a standard of practice.”
20 June, 18:50 BST
Benefit-risk consideration regarding paclitaxel devices is discussed amongst the panel. Citing a significant number of sources and data demonstrating clear benefit, with the meta-analysis “on the other side of the scale” demonstrating risk, Todd Rasmussen maintains that while the meta-analysis was “extremely well done and is highly important, […] continued marketing of the paclitaxel-coated devices for patients with symptomatic SFA disease should be allowed.”
Joaquin Cigarroa similarly argues that paclitaxel provides a proven “very consistent and clinically profound benefit” to a patient population that greatly needs it. Krucoff adds to this point that the patient perspective is at the centre of this discussion of weighing up the benefits and the risks. He says, “how to clarify the risk and what the risk really is—I think that conversation really needs to go forward.” Several comments across the panel agree that the conversation with patients clarifying these risks and guiding them to weigh up short-term and long-term impacts effectively, underlining that patient agency and choice should be available. Philip Posner further highlights that from his personal perspective, “when you talk to the patient, you have to have the patient learn what the risk really is, what can be done to modify that risk, and then what is the reward.”
Nevertheless, John Hirshfeld argues that the FDA “cannot just walk away from this and say it is ok”, but rather provide some real guidance and continue to collaborate on this issue.
John Somberg states “I don’t think anyone is talking about taking the device off the market. The question most concerning the signal is the risk-benefit ratio.”
20 June, 19:30 BST
With regards to post-market studies and surveillance, the FDA panel reviews the recommended objectives of future trials, what data should be collected, study endpoints and study design.
Karla Ballman emphasises to this point, “I do not think the registries that are in place or the Medicare data are adequate for assessing sort of the signal long term, just because of all the biases in there.” Panel members further stress the importance of intervening in ongoing trials, to highlight the importance of follow-up to five years rather than a one-year endpoint.
“I think there are 21st century way of going forward”, Krucoff says, “is collaboratively using registry-based prospective randomization if that was the best fit. That would ease the burden, increase the speed, reduce the cost, even share the cost, and whatever device is used, let it be used.”
John Somberg points to SWEDEPAD and the potential significant data this trial could provide, once enrolment resumes. Karla Ballman and Mitchell Krucoff both put forward that the quickest, most cost-effective way to gain more insight is by pushing for current ongoing prospective registry trials and other studies to attempt to close the gap of missing data.
Richard Lange summarises, there are data that are available already which has some limitations, from randomised controlled trials. In addition, “there are studies that are either just initiated or ongoing, and I would push those studies to get the information we need, primarily mortality data is what we’re interested in, so long-term follow up. I’ve heard the word collaboration from everybody in the panel. And from industry as well. Because I don’t think anyone wants to tackle this or can tackle it by themselves.”
He adds that importantly, the opinion on the value of registry-derived data is varied across the scientific community.
20 June, 19:50 BST
Discussing potential modifications to labelling of approved paclitaxel devices, Bram Zuckerman asks, “how can we update the labelling, in a transparent fashion that will be of use to practicing physicians and patients who read the label?”
Joaquin Cigarroa responds, the labelling must incorporate the sentiment that “there may—not that there is—a late mortality signal, should be included.” John Somberg contends, however, that a long and non-unidirectional message showing the totality of data would not be read by physicians, and not understood by patients. Instead, Somberg states “if we think there is a signal”, the label should read “something simple in layman’s terms that uses the word ‘may'”.
20 June, 20:00 BST
The panel discusses specific study designs to better evaluate paclitaxel devices for PAD. Firstly, the panel agrees that studies “should not end at 12 months”, but rather continue to collect data out to three or five years.
Zuckerman clarifies, “What we’re asking is for a new PMA device, given what you said, you would wait until we have five years safety results for a new paclitaxel drug-eluting stent.” Ballman responds that while one year is acceptable to determine benefit and efficacy, safety needs to be assessed with long-term follow-up. Cigarroa adds, “I would follow under one year for efficacy, with additional teeth, and attention to the detail of ascertainment to subsequent clinical events with a methodology and an adjudication process that we can feel confident through five years.”
To this point, Lange underlines the “teeth” required, to ensure the data is collected and distributed rigorously to regulatory bodies.
Furthermore, the Todd Rasmussen suggests that as dosing mechanism understanding is evolving, future studies may need to separate DCBs from DES. Kevin Kip meanwhile states that “Any new study must place a premium on paclitaxel exposure prior to the index procedure, and after the index procedure, so that you know that over the course of time and follow-up, who was exposed and who wasn’t.” Kip further adds that adjudication must be added into budget consideration, as it is a time-consuming and costly, but important, effort.
Bram Zuckerman states, “Unfortunately, we have a signal here that remains undetermined. One of the reasons why is that the death adjudication uniformly in these FDA trials was poor.” He summarises, “going forward, mortality will be given a higher priority, and we will need to think about how it can be best assessed and adjudicated.”
Finally, Zuckerman suggests, “I think the basic thing that we’re looking at in this question is a whole rethink of the clinical trial design and execution in this field potentially making it more uniform, which should add efficiencies and better understanding of the data.” Todd Rasmussen agrees “we need to think of new creative ways to do clinical studies in the future”, and produce common data elements.
20 June, 20:25 BST
Based on the available data, the panel discusses whether their recommendations may be applicable to paclitaxel devices with other indications for use. Responding, John Somberg reiterates the importance of analysing efficacy at one year and safety follow-up of three to five years.
With regards to dialysis and CLI patients, the panel suggests that benefit-risk considerations “may be different” for these populations, either because of mechanism or because of longevity of the patient populations affecting risk tradeoffs. Nevertheless, Lange underlines that providing thorough information to the patient is essential to informed consent and patient choice.
Concluding the meeting, Bram Zuckerberg states that the two-day meeting and presentation has been “extremely helpful” for the FDA, who will now consider the analysis of the panel, and “look forward to continued collaboration in this field.”










