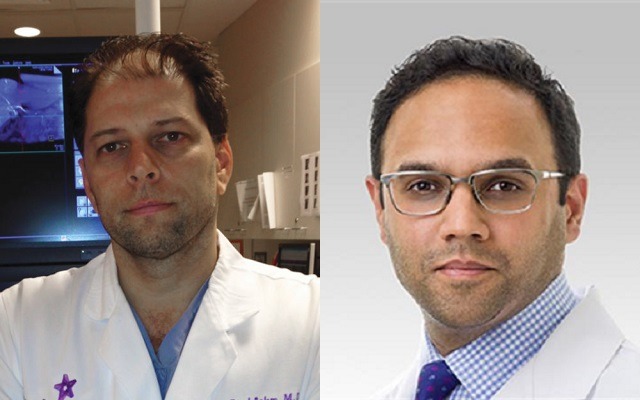
The support of the UK’s National Institute for Health and Care Excellence (NICE) signals that embolization has a unique role in the treatment of benign prostatic hyperplasia, outside of the traditional spectrum of medical and surgical options, write Riad Salem and Samdeep Mouli, Chicago, USA, while reviewing the new evidence in favour of the minimally invasive procedure.
Benign prostatic hyperplasia affects more than half of men over the age of 50 and its incidence increases with age. Enlargement of the prostate gland leads to lower urinary tract symptoms (LUTS), including urinary frequency and urgency, nocturia, difficulty urinating, and incomplete bladder emptying. Together these symptoms lead to a significant impairment to quality of life. Management of these symptoms can be challenging, and must take into account prostate disease burden, pre-existing sexual function, and medical co-morbidities.
Several medical and surgical therapies have been utilised to treat this patient population, but variable efficacy and persistent side effects have driven patients to seek alternative therapies that maximise quality of life. As such, the treatment of these symptoms has evolved over the last several years, moving away from invasive surgical options towards minimally invasive therapies. Concurrently, a greater emphasis has been placed on functional outcomes and quality of life, such as hospital stay, recovery time, and return to work. Prostate artery embolization has been developed to address these limitations of current treatment options. Via imageguided catheter-directed embolization of the prostatic arteries, embolization induces ischaemic necrosis of the gland, with resultant improvement in LUTS.
The initial prostate artery embolization studies focused on understanding arterial anatomy, defining patient selection, and demonstrating technical feasibility. These early studies demonstrated safety and efficacy, with a relatively favourable side-effect profile, mostly limited to mild transient haematuria and dysuria. Critically, multiple studies have confirmed that embolization does not result in the typical urinary and sexual dysfunction issues seen with both medical and surgical treatment options.
Early enthusiasm for this novel therapy was tempered by technical difficulty. Initial variability in clinical outcomes has subsided with refinements in microcatheter technique, embolic agent selection, a clearer understanding of arterial anatomy, as well as the advent of cone-beam CT. Along with these advancements, more mature data has emerged clarifying the role of embolization in the treatment of lower urinary tract symptoms, secondary to benign prostatic hyperplasia.
Within the last year, several studies have demonstrated efficacy across prostate gland sizes, particularly in patients with large prostates (>80 grams), which are often difficult to treat surgically. Additionally, embolization has been successfully employed to treat hyperplasia-related chronic urinary retention requiring long-term foley catheterisation. Several groups have reported 80–90% of patients with chronic urinary retention are catheter-free following embolization. Critically, the procedure has been proven safe and effective in patients who are not surgical candidates due to underlying medical co-morbidities.
Data from the multicentre UK ROPE (Registry of prostate embolization) registry of prostate artery embolization have recently been published by Alistair F Ray and colleagues in BJU International in April 2018. Investigators compared 305
patients undergoing embolization (n=216) vs. the surgical gold standard, transurethral resection of the prostate (TURP; n=89) in the setting of a noninferiority study. While embolization did not outperform TURP, significant improvements in both urinary symptoms and quality of life were observed, without significant complications or effects on sexual function. Additionally, the majority of patients in the embolization arm were treated on an outpatient basis, whereas surgical patients required at least overnight admission. The results of this registry mirror our own US FDA-approved prospective open label trial presented at the Society of Interventional Radiology’s 2018 meeting (SIR; 17–22 March, Los Angeles, USA). In a cohort of 45 men treated with embolization, we observed early and sustained improvements in urinary function and quality of life over a one-year follow-up period. There were no severe complications, and sexual function was not affected throughout the course of the study. These data are currently under review.
These latest studies add to the data proving embolization is both safe and effective for treating lower urinary tract symptoms secondary to benign prostatic hyperplasia. It offers significant and sustained improvement to both urinary function and quality of life. This body of evidence has led the UK’s National Institute for Health and Care Excellence (NICE), the governing body for health and social care, to support the use of embolization in the National Health Service (NHS). NICE does not usually approve new treatments without significant reflection and a critical review of the data; their approval of embolization into the treatment algorithm is sure to set the stage for reimbursement approval in the USA. The support of the UK’s NICE signals that embolization has a unique role in the treatment of benign prostatic hyperplasia, outside of the traditional spectrum of medical and surgical options.
Moving forward, the treatment of benign prostatic hyperplasia and lower urinary tract symptoms will require multidisciplinary collaboration, tailoring treatment to both patient disease burden and functional goals. In this context, embolization should be offered to patients seeking an alternative to current therapies, one which maximises quality of life. In 2014, we predicted that embolization would become one of the standard of care treatments for benign prostatic hyperplasia within three to seven years after data from Portugal and Brazil could be confirmed in independent cohorts. The work of Nigel Hacking and the other UK investigators, has helped to accomplish this feat in four years.
Samdeep Mouli and Riad Salem are both at the Section of Interventional Radiology, Northwestern University, Chicago, USA. They have reported no disclosures pertaining to this article.