Is there a relationship between neovascularisation and pain? If so, embolization has the potential to change the way we think of treating chronic pain, say Sandeep Bagla and Rachel Piechowiak in an article describing the use of geniculate artery embolization to treat osteoarthritis.
More than 25 million people in the USA suffer from osteoarthritis, with the knee joint being the most common site. The mainstay of treatment for mild and moderate pain is medical therapy, with non-steroidal anti-inflammatory drugs (NSAIDs). Unfortunately, NSAIDs can be a cause of renal failure, exacerbation of asthma and most notably, gastrointestinal haemorrhage. The estimated number of deaths from NSAID-related gastrointestinal bleeding is 16,5001. Hyaluronic acid injections and platelet-rich plasma injections have been used with variable success. When medical therapy and intra-articular injections fail, surgery is the last option. Patients who are resistant to medical therapy but do not have osteoarthritis severe enough to warrant a joint replacement are a unique and challenging group to treat.

Genicular artery embolization is a promising, minimally invasive therapy that has been shown in early studies to have significant and lasting symptom relief in patients with mild to moderate osteoarthritis. This is an extension of previously reported success with embolization in the settting of haemarthrosis2. The rationale for genicular artery embolization in patients with osteoarthritis is based on the idea that angiogenesis occurs where there is chronic inflammation. In patients with osteoarthritis, chronically inflamed synovia usually result from a combination of altered biomechanics, joint trauma, age, obesity, and an immune/inflammatory mediated response. Cytokines such as vascular endothelial growth factor (VEGF), are released that induce angiogenesis. The newly formed blood vessels grow into the cartilage, synovium and adjacent bone, bringing with it new sensory nerve fibres. This neovascularity is felt to perpetuate more inflammation, cartilage and bone destruction, as well as development of osteophytes. It is postulated that by embolizing the abnormal increased vasculature in the inflamed synovium, the intricate relationship between angiogenesis, chronic inflammation and pain is disrupted, thereby decreasing symptoms and possibly delaying further joint derangement3.
A series of small studies led by Yuji Okuno4 has changed the way we are thinking of pain and embolization. Initially reporting on elbow tendinopathy and shoulder capsulitis, Okuno and colleagues subsequently published their experience performing geniculate artery embolization in 14 patients with painful knee osteoarthritis. Particulate embolizaton was performed with either an antibiotic or a 75 micron spherical embolic in the region of palpable pain, after identifying an area of synovial hypervascularity. Overall, patients experienced a significant reduction in knee pain and disability.

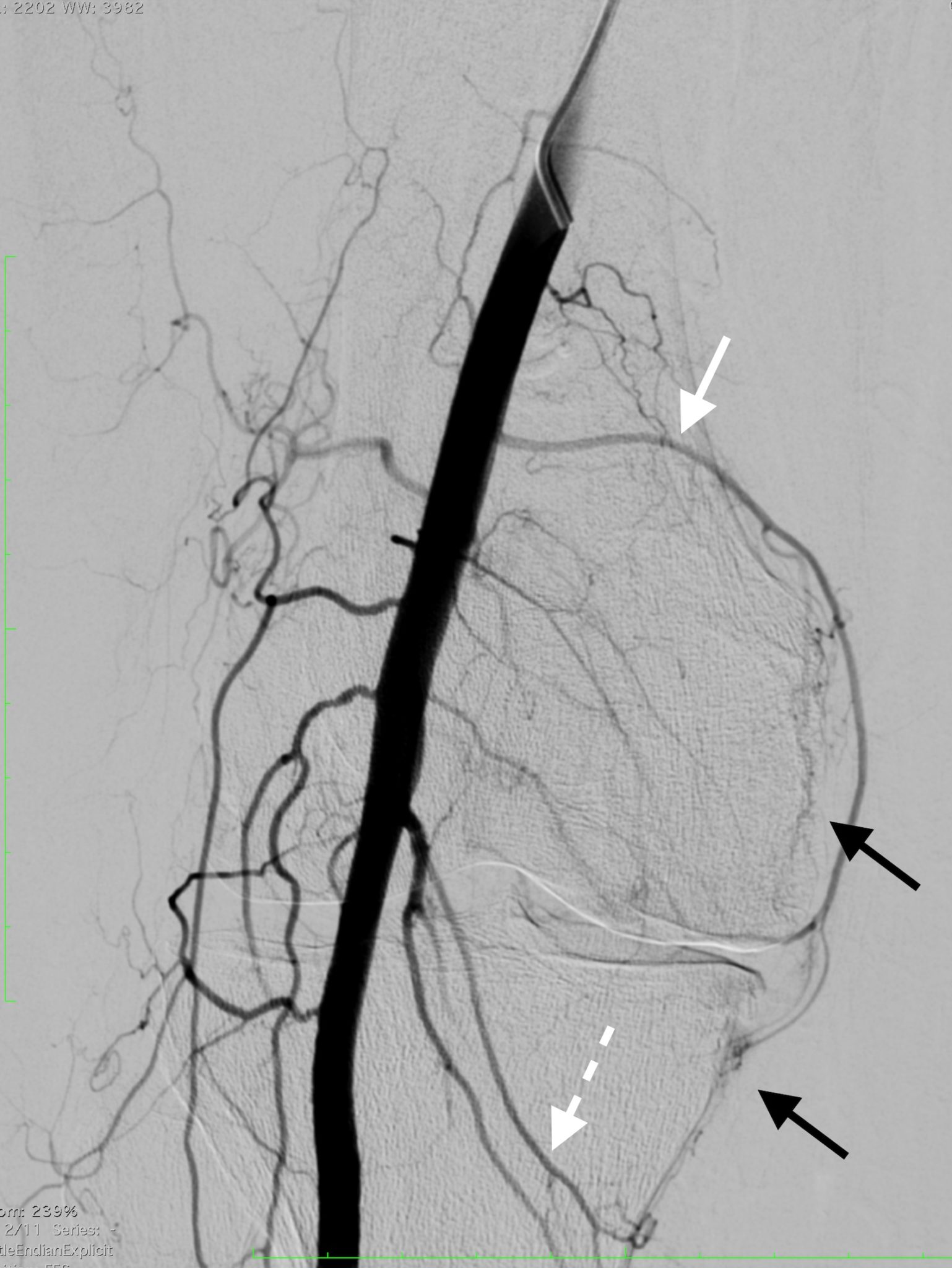
This summer, a South American pilot study has been initiated between the authors and Ricardo Garcia-Monaco at the Hospital Italiano in Buenos Aires, Argentina. Thus far, five patients with intractable knee pain have undergone geniculate artery embolization using 75 micron spherical embolic in the region of palpable tenderness. Patients also underwent preoperative MRI with contrast to evaluate for areas of increased synovial enhancement (Figures 1 and 2). Continued enrolment and long-term assessment of pain control is ongoing.
Further, in the USA, Sandeep Bagla and Ari Issacson have received approval for an investigational device exemption study for geniculate artery embolization. This single-arm, 20-patient, study is expected to initiate enrolment in the autumn of 2016 at University of North Carolina at Chapel Hill. The endpoints for this study will include reduction in pain, disability and the requirement for escalation of therapy.
We are in the midst of an embolization renaissance. Advancements in the interventional community are leading to new applications for embolization, including pain, cancer, obesity and prostate disease. The future of interventional therapies looks exciting…
Sandeep Bagla is adjunct associate professor, UNC Chapel Hill, Vascular Institute of Virginia, Woodbridge, USA. Rachel Piechowiak is with Vascular and Interventional Radiology, Vascular Institute of Virginia, Woodbridge, USA.
References
1 Singh, G. Gastrointestinal complications of prescription and over the counter nonsteroidal anti-inflammatory drugs: A view from the ARAMIS Database. American Journal of Therapeutics 2000; 7: 115–121.
2 Weidner ZD, Hamilton WG, Smirniotopoulos J, Bagla S. Recurrent hemarthrosis following knee arthroplasty treated with arterial embolization. Journal of Arthroplasty 2015; 30:2004–2007.
3 Walsh DA. Angiogenesis and arthritis. Rheumatology 1999; 38:103–112.
4 Okuno Y, Korchi AM, Shinjo T, Kato S. Transcatheter arterial embolization as a treatment for medial knee pain in patients with mild to moderate osteoarthritis. CardioVascular and Interventional Radiology 2015; 38:336–343.