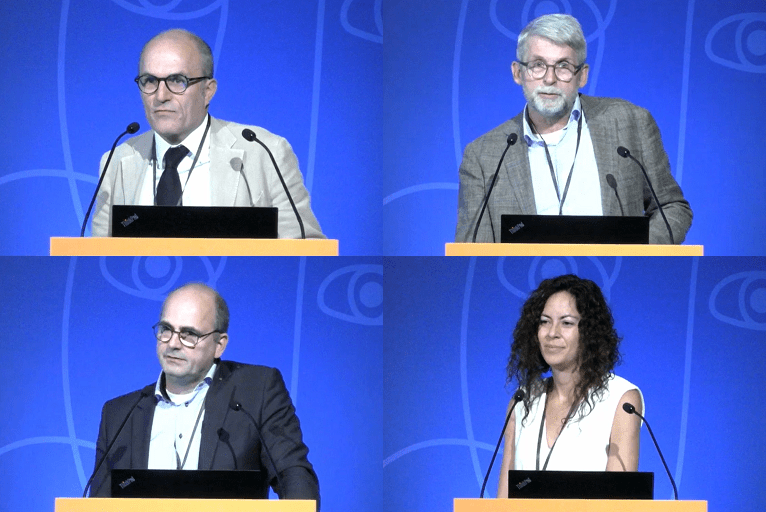
The management of renal cancer patients featured prominently at this year’s Cardiovascular and Interventional Radiological Society of Europe (CIRSE) annual meeting (10–14 September, Barcelona, Spain), with discussions around patient selection and treatment planning preceding talks on the key therapeutic options in this space.
The first of four presentations was delivered by Rosario Grasso (Campus Biomedico University Hospital Foundation, Rome, Italy), who argued that percutaneous thermal ablation approaches like radiofrequency ablation (RFA) or cryoablation are an option for the management of patients with clinical-stage T1 renal lesions—primarily in masses <3cm in size, but potentially for larger masses in select patients too.
Grasso stated a belief that percutaneous ablation represents a safe and effective alternative to surgery in treating T1a renal cell carcinomas due to the “excellent” functional and technical outcomes seen with the procedure. The “very low” complication rate these procedures hold also compares favourably to those associated with nephrectomy, he added.
The speaker concluded that there is currently Level C evidence that, in selected patients with suspected T1a renal cell carcinoma, percutaneous thermal ablation should be offered over active surveillance owing to the “acceptable” long-term oncological and survival outcomes it has demonstrated to date. Grasso also said RFA, cryoablation and microwave ablation are all appropriate treatment modalities, and claimed that the choice of ablation method “should be left to the discretion of the operating physician”.
Treatment planning
Arian van Erkel (Leiden University Medical Center, Leiden, The Netherlands) followed this by discussing treatment planning in renal ablation—a “well-established” treatment for small T1a tumours. He posited that the first step here is to choose between surgery, ablation or active surveillance, and that this decision is an individualised one influenced by patient preference, age and life expectancy, renal function, the location and size of the tumour, and multiple other factors.
“Planning the treatment of your RFA is very important in getting complete ablation, with a sufficient margin, and in avoiding complications,” van Erkel asserted. “This planning involves image guidance, the ablation modality and protective measures.” He further claimed that axial diameter, bowel proximity, adjacency to the ureter, and several other characteristics of the tumour, should be taken into account.
“An immediate CT [computed tomography] after ablation is, of course, important, to evaluate your complications and your ablation margins especially,” van Erkel concluded. “And, there is software on the market that can help you make these estimations in a more scientific and exact way.”
Different modalities
A closer look at the different approaches to percutaneous ablation for renal cell carcinoma was then provided by Esther Gálvez González (Hospital Severo Ochoa, Madrid, Spain). The speaker corroborated many of her colleagues’ earlier points, noting that ablative treatment is as effective as surgery in T1a tumours—adding that it can also help to preserve renal function, and is associated with low complication rates.
Gálvez González further asserted that a key advantage held by RFA is the wealth of experience and high volume of published papers associated with the technique, but also noted two important limitations: thermal tissue conductivity and the ‘heat sink effect’. In contrast, she continued, bigger tumours can be ablated more quickly, and at higher temperatures, with microwave ablation, while its relative insensitivity to the heat sink effect allows it to be used in target areas located closer to larger blood vessels. The major limitation of microwave ablation, however, is the increased risk of complications in more central locations, which restricts its use to peripheral lesions, she added.
The speaker also touched on the various advantages and limitations of two other approaches—cryoablation, and a non-thermal technique (on which there are minimal published data) called irreversible electroporation—stating that both are essentially unaffected by impedance and the heat sink effect, but are limited by smaller ablation volumes and longer procedure times as well. Gálvez González concluded by asserting the importance of selecting the correct approach based primarily on the size and location of the target tumour.
Combined therapies
The session’s final talk was given by Marco van Strijen (St Antonius Hospital, Nieuwegein, The Netherlands), who outlined several combined treatments in cryoablation. “Combined treatment in renal cryoablation, in my opinion, consists of either embolization—which is a safe treatment but for which scarce literature is available—or thermoprotection by liquid; air or CO2 dissection; or pyeloperfusion,” he stated. Homing in on the former technique, the speaker said that, despite the limitations around previous studies and a lack of prospective data, percutaneous embolization is considered a safe procedure that is “most effective” in reducing periprocedural blood loss, and holds potential benefits in local tumour control and procedural visibility.
Van Strijen went on to highlight two further, more recently introduced tools that he also considers among the options for combined approaches: robotic needle placement, and the use of integrated controls and augmented reality to perform ablations virtually with the aid of a HoloLens device (Microsoft). In concluding his presentation, van Strijen added: “Robotic needle placement is currently one of my favourite techniques.” Here, he cited the fact it is “very simple”, and enables steep angulations, as well as reducing radiation exposure and speeding up the procedure “considerably”.