While emphasising the interesting findings from their laboratory for interventional radiologists, Olivier Jordan and Katrin Fuchs write that laboratory benches not only give birth to inventions with a potential for translation into clinics, but also contribute to unbiased characterisation of products already in clinical use.
In 2007, sorafenib received FDA approval as a systemic treatment of patients with unresectable hepatocellular carcinoma, after conventional chemotherapeutic drugs had not shown efficacy for this indication. Sorafenib suppresses several molecular targets involved in the establishment of vessels toward tumors. A series of clinical phase III trials were conducted with other oral anti-angiogenic agents; however, none has since provided the same treatment outcomes as sorafenib in terms of efficacy and safety.
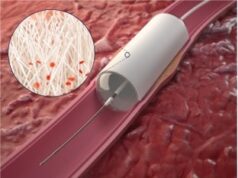
The toxicity related to systemic distribution of a drug in the body might be overcome by a local administration approach, such as drug-eluting beads (DEBs) used during transarterial chemoembolization (TACE). Furthermore, the anti-angiogenic activity of these drugs should be especially beneficial after TACE, where growth factors are released in response to the ischaemic and necrotic conditions, which in turn, triggers endothelial cell proliferation and migration into new blood vessels.
In a laboratory, we can evaluate the feasibility of loading therapeutic doses of a chemotherapeutic or anti-angiogenic drug onto embolic beads. For the small molecules doxorubicin, irinotecan, and sunitinib, the procedure is relatively easy, since the drugs are protonated, allowing loading by soaking the beads in the drug solution. Even the anti-angiogenic antibody bevacizumab, although of higher molecular mass and less stable, can be loaded on beads via this mechanism. Sorafenib, in contrast, requires more complex and challenging loading techniques due to its very low solubility and neutral charge. Drug loading on commercial beads remains to be optimised. However, several research groups have already successfully explored the encapsulation of the drug during the fabrication process of their home-made beads. By chromatographic and spectroscopic methods, the kinetics and the capacity of loading of a drug are precisely determined and thus the system well characterised, to be able to deliver predictable drug concentrations.
Once the beads are loaded with a drug, the drug elution kinetics from the embolic beads can be assessed in the laboratory. The so-called in vitro release methods are commonly employed in the pharmaceutical industry in order to measure drug release from a carrier. This may be any pharmaceutical form such as a tablet, or a drug-eluting bead. The advantage of these methods and apparatus is their standardisation beyond laboratories, which allows for comparisons, provided that the same parameters and release media are used. First, the in vitro release techniques allow for comparison of elution of different drugs from the same type of beads. For instance, doxorubicin-eluting beads and sunitinib-eluting beads differ strikingly in terms of the drug release kinetics and amount of released drug under similar conditions (flow speed, release medium). Second, the same drug loaded on different type of embolic beads often results in a different elution pattern due to weaker or stronger interactions with the bead polymer. In this way, properties of embolic beads from various producers can be checked and characterised by an independent intermediate laboratory, quickly and at low cost before blind in vivo experiments.
Depending on the geometry of the in vitro apparatus, different drug release kinetics and extent of drug release are obtained, which underlines the importance of the flow during drug elution. In an embolized vessel, little or no flow can be expected, thus decreasing the speed of drug elution. Also, the residence time of drugs like doxorubicin, sunitinib, and sorafenib in the liver tissue is much longer than predicted in vitro due to protein and tissue binding. Consequently, correlations of the in vitro release with in vivo concentrations remain a complex aspect. Often, plasma concentrations instead of local concentrations are considered for the correlation, although plasma levels should actually remain low with the local delivery. For this reason, local biodistribution measurements in the tumour as well as in adjacent untreated tissues are needed to assess drug pharmacokinetics. Chromatographic and imaging methods have been developed for this purpose.
Novel biodegradable beads have been designed in various labs and combined with anti-angiogenic drugs. The interplay of degradation and elution kinetics is a promising but still poorly understood approach to deliver the drug efficiently at the right time after the embolization procedure, when growth factor levels peak. Finally, MR or CT-imageable DEBs are under evaluation, which may provide a better prediction of drug elution and distribution in the target organ.
In summary, the laboratory benches do not only give birth to inventions with a potential for translation into clinics, but also contribute to unbiased characterisation of products already in clinical use, and may ultimately offer a deeper understanding of local drug pharmacokinetics in the targeted tumour tissues.
Olivier Jordan is a senior scientist and senior lecturer at the School of Pharmaceutical Sciences, University of Geneva-University of Lausanne, Geneva, Switzerland. Katrin Fuchs is a PhD candidate and licensed pharmacist at the same institution. The authors disclose that a patent has been filed on the subject. The Leman Research Group from Lausanne, Switzerland has been awarded CIRSE’s 2015 Award of Excellence and Innovation in interventional radiology for their research on drug-eluting beads loaded with anti-angiogenic agents for chemoembolization, particularly for the research project “sunitinib-eluting beads”. In addition to the two authors above, the Leman Research Group consists of Alban Denys, head of the Digestive and Oncologic Imaging and Interventional Radiology Unit, University Hospital of Lausanne (CHUV); Pierre Bize, senior physician, Department of Medical Imaging at CHUV and Gerrit Borchard, professor in biopharmaceutical sciences at the University of Geneva.