The ‘Connect the world: Japan’ session at this year’s Leipzig Interventional Course (LINC 2023, 6–9 June, Leipzig, Germany)—in collaboration with the Japanese Endovascular Treatment Conference (JET)—sparked discussion surrounding the latest data in femoropopliteal interventions. Giving platform to multiple first-time data releases, the LINC 2023 audience were presented with awaited updates from global trials.
Stepping up to the podium first, Marianne Brodmann (Medizinische Universität Graz, Graz, Austria) presented the initial Ranger superficial femoral artery (SFA) II randomised controlled trial (RCT) three-year patency and four-year clinical safety results. This study compared the Ranger drug-coated balloon (DCB; Boston Scientific) plain balloon angioplasty.
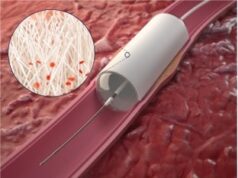
The study aimed to evaluate the safety and effectiveness of the Ranger DCB (paclitaxel dose density 2μg/mm2) for treating SFA or proximal popliteal artery lesions—Brodmann explaining briefly that paclitaxel-coated balloon treatment prevents reinterventions however dosage and coating characteristics can differ, affecting efficacy determination.
Regarding their cohort demographics and clinical history, Brodmann noted there was no major differences between study arms, however around 40% of patients were identified as having diabetes. Lesion characteristics were also similar between groups—mean lesion length Brodmann addressed as being not statistically significant, although a higher degree of calcium was found in the plain balloon arm. Additionally, she added that there was a higher percentage of total occlusion in the plain balloon arm.
Summarising their long-term outcomes for the LINC 2023 audience, Brodmann highlighted the three-year primary patency of DCBs at 177.4% over plain balloon angioplasty at 73.5%—“in comparison to other DCB trials out there, our three-year primary patency is much higher” she concluded. Turning to outcomes concerning major amputation and four-year mortality rates, they found no significant difference in all-cause mortality and amputation in both arms. However, when regarding four-year efficacy data, Brodmann stated that the DCB provided higher freedom from clinically driven target lesion revascularisation (CD-TLR) at 78.7% compared with 74.5% for the plain balloon arm.
Concluding her presentation, Brodmann observed that their study “demonstrated outstanding three-year primary patency of 77% for the low-dose paclitaxel DCB and four-year freedom from CD-TLR which is greater than those reported in other DCB studies previously published”.
Brodmann later returned to the podium to deliver another first-data release from the ELEGANCE registry, the purpose of which was to collect real-world data from underrepresented minorities (URMs) and women who have “previously not been represented” in peripheral arterial disease (PAD) trials. The aim of this registry, Brodmann summarised, is—as the trial is ongoing—to examine variation in treatment among sociodemographic groups for those treated with DCBs.
The registry has recruited 566 subjects across 31 sites, in three countries/regions to date which have been treated with the Ranger DCB. Expanding on patient demographics, Brodmann stated that theirs is a complex subject cohort due to the “higher prevalence” of chronic limb threatening ischaemia (CLTI) in Black and Hispanic patients, longer lesion length in Black subjects, while 61.1% of patients were identified with moderate/severe calcification.
Of their conclusions to date, Brodmann conveyed the higher burden of atherosclerotic risk factors faced by women and URMs, and that baseline clinical characteristic differences between sex and race/ethnicity groups suggest variability in time to diagnosis, treatment planning and access to care.

Next, reporting on the four-year results from the TINTIN trial investigating the combination of the Luminor DCB with the iVolution bare metal stent (both iVascular). Koen Deloose (AZ Sint-Blasius, Dendermonde, Belgium) gave a brief description of the study, which was performed in nine centres and enrolled patients who had TASC C or D lesions that were more than 150mm in length. Similar to Brodmann et al’s research, Deloose and his team defined their primary endpoint to be freedom from CD-TLR at one year, with a follow-up period of up to five years.
Presenting the 48-month results of the TINTIN trial, Deloose outlined that in the 100 patients in their cohort 72% were claudication patients and 28% chronic limb-threatening ischaemia (CLTI) patients. The mean lesion length in this group was 24cm. Additionally, they identified occlusions in 60% of patients and 70% had severe calcification. At 48 months, Deloose noted that they have had 36 deaths and some withdrawals/missed visits, so their current data is drawn from the 52 remaining patients.
“In terms of survival, you notice how diseased this vascular population is with lesions up to 24cm—in the CLTI patient group we saw a survival rate of 61% at four years, which I think is completely in line with findings in the literature,” Deloose opined. The reasoning for this outcome, he continued, is due to a “heterogeneous group of causes, which are not related to procedure, nor device”.
Freedom from major adverse events (MAEs), CD-TLR or major amputation was found to be 44.6% at four years, while they have identified 19 CD-TLRs and a single case of major limb amputation in the CLTI group. Deloose stated that they reached their 30-day primary safety endpoint without any occurrence of an event.
Moving on to consider freedom from CD-TLR more closely when using this combination therapy, Deloose posited that, at four years, they saw “quite good results” showing freedom from CD-TLR to be at 75% in the remaining population—”this means three out of four did not have reintervention if they were still alive at four years”.
Comparing their results with similar studies, Deloose confirmed that theirs data are in the “same area”, and that the TINTIN trial shows the “durability of a combination of an efficient DCB and scaffolding in the most complex lesions”.

Subsequently presenting another first-time data release, (Ziekenhuis Oost-Limburg, Genk, Belgium) delivered results from the REGAL registry—a real-world, all-comer study comparing the Eluvia DCB (Boston Scientific) and bare metal stents. The study concerned patients aged 80 or older, with Lansink emphasising that this means they have received “all kinds of treatments”. Furthermore, he made a clear note that “these are very ill patients”, with lesion lengths of up to 10cm and a 50% chronic total occlusion rate.
“The Kaplan Meier primary patency projection through to 12 months was 92%” Lansink observed, “which is of course very good looking ahead to 24 months.” He also emphasised the durability of primary sustained clinical improvement at 24 months, which is a “good sign for these kind of stents”. Additionally, major amputation rates remained low in the patient population and was recorded as 2.2% at 24 months.
Summarising their findings for the LINC 2023 audience, Lansink restated that this is real-world data pulled from patients with complex lesions, high rates of chronic total occlusion and high rates of diabetes. Despite the high-risk nature of their population, at 12 and 24 months the Kaplan Meier primary patency rates were 92% and 83%, respectively, Lansink confirmed. Freedom from CD-TLR was recorded as 93% and 88%, while sustainable clinical improvement was seen in 83% and 81% of patients at 12 and 24 months.
“Collectively, the data demonstrates the safety and efficacy of the Eluvia stent in SFA, proximal popliteal lesions and even in a population with advanced peripheral arterial disease and a higher occurrence of comorbidities,” Lansink conveyed.