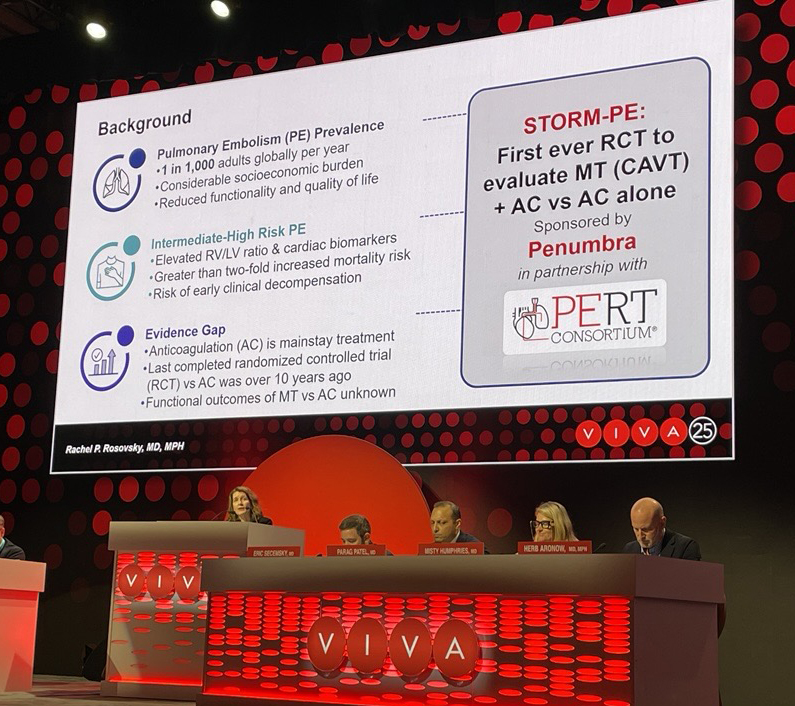
Mechanical thrombectomy by means of computer-assisted vacuum thrombectomy (CAVT) using the 16Fr Lightning Flash system (Penumbra) along with anticoagulation for acute-to-intermediate pulmonary embolism (PE) demonstrated functional assessment improvements, earlier physiological recovery and greater reduction in pulmonary artery obstruction when compared to anticoagulation alone. These were among the latest findings from the STORM-PE randomized controlled trial (RCT) presented today at the 2025 Vascular Interventional Advances (VIVA) conference (November 2–5; Las Vegas, USA).
STORM-PE data were first presented at 2025 Transcatheter Cardiovascular Therapeutics (TCT) conference (25–28 October, San Francisco, USA), where it was revealed that CAVT with anticoagulation achieves superior reduction in right heart strain compared to anticoagulation therapy alone. The trial, which enrolled 100 patients across 22 international sites, showed that patients treated with CAVT demonstrated a greater reduction in right-to-left ventricular (RV/LV) diameter ratio within 48 hours (mean reduction 0.52 vs. 0.24; p<0.001) and nearly 80% of patients had positive treatment effect with CAVT, which was significantly greater than the patients who received anticoagulation alone (78.3% vs. 51.9%; p=0.011), reflecting rapid haemodynamic recovery. The primary results from the study were published today in Circulation.
“The latest STORM-PE findings demonstrate substantial improvements in both clinical and functional outcomes, with a significantly higher proportion of patients treated with CAVT plus anticoagulation returning to normalization within 48 hours compared to anticoagulation alone—a remarkable result,” said presenting author Rachel Rosovsky (Harvard Medical School, Boston, USA), co-global principal investigator of STORM-PE. “STORM-PE highlights the critical importance of early intervention in patients with intermediate-high risk PE and provides the strongest evidence to date that advanced therapy with CAVT offers superior efficacy compared to the current standard treatment of anticoagulation alone. These breakthrough results not only advance the field but also have the potential to meaningfully improve patient care and recovery.”
In the trial, patients treated with CAVT plus anticoagulation experienced significantly lowered thrombus burden at 48 hours, with a 2.7 times larger reduction in refined modified Miller score (42.1% vs 15.6% relative reduction; p<0.001), Rosovsky reported.
They also saw early physiological recovery with significantly lower heart rate (80.0bpm vs 86.4bpm; p=0.022) and less tachycardia (heart rate >100, 2.2% vs 20%; p=0.008), reduced supplemental oxygen requirements (0.5L/min vs 1.4L/min; P = 0.027), and a lower National Early Warning Score-2 (NEWS2) risk of clinical deterioration (1.8 vs 2.7; p=0.034) at 48 hours.
CAVT-treated patients experienced 2.2 times greater likelihood of progressing towards recovery of functional status, based on post-venous thromboembolism functional status (PVFS) from pre-PE event to discharge (p=0.032); as well as significantly longer distance walked during the 90-day six-minute walk test (472m vs 376m; p=0.019). Additionally, Rosovsky said, CAVT patients near normalized by 90 days, walking 94% of their predicted walk distance versus 75% among the patents treated with anticoagulation only (p=0.022). Safety rates through 90 days were comparable, she added.
“STORM-PE is the first RCT to report the results of mechanical thrombectomy with anticoagulation versus anticoagulation alone. The CAVT arm demonstrated superior reduction in RV dilatation and a similar safety profile to the AC arm,” Rosovsky told VIVA 2025. “These promising results reinforce the role of mechanical thrombectomy, specifically CAVT, as an effective treatment strategy in patients with acute intermediate-high-risk PE.”
Immediately prior, John Moriarty (UCLA Health, Los Angeles, USA) delivered one-year functional and quality-of-life (QoL) outcomes from the STRIKE-PE study, a single-arm, prospective, multicentre, ongoing trial looking at CAVT patients treated using the 16Fr catheter.
Results from the trial show that mean RV/LV ratio decreased from 1.34 at baseline to 0.95 at 48 hours—a 27.3% decrease (p<0.001), he said. The composite major adverse event (MAE) rate was 0.8% (two patients).
All functional outcomes were improved at one year: median Borg dyspnea scale at rest improved, decreasing from 4 at baseline to 0 (p<0.001), mean 6-minute walk test distance increased from 222.5m at discharge to 370.7m (p<0.001), and the New York Heart Association (NYHA) classification distribution recovered to that before the PE event.
Moriarty said multiple QoL measures showed gains—notably, mean total PEmb-QoL improved, decreasing from 43.7 at baseline to 14.2 at one year (p<0.001), a continued improvement from the 90-day result (p<0.001).
“These findings demonstrate that treatment with CAVT using the 16F catheter system enhances patient outcomes and potentially reduces the long-term burden of PE-related sequelae,” he concluded.