First expected in late 2025, the UK National Health Service (NHS) 10-year cancer plan, setting out a comprehensive strategy for oncology funding and care coordination, has been delayed and is expected for release in early 2026. Clinicians now wait for further updates amid new reports which state approximately three out of 121 NHS Trusts are meeting waiting time targets and, according to a recent publication in The Lancet by journalist Elizabeth Gourd, additional delays to the release of the plan could cost lives.
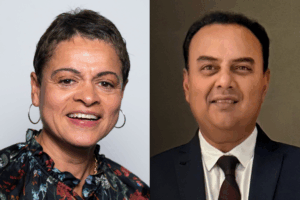
Nicky Thorp (The Christie NHS Foundation Trust, Manchester, UK), vice president of clinical oncology at the Royal College of Radiologists (RCR) and Praveen Peddu (King’s College Hospital, London, UK), chair of the Interventional Oncology United Kingdom (IOUK) group, speak to Interventional News on what must be factored into the awaited plan to strengthen the NHS’s cancer care system.
Bureaucratic barriers
Thorp uses the example of stereotactic ablative radiotherapy (SABR) to illustrate how “bureaucratic hurdles” throughout the commissioning process—despite being placed in “good faith”—are stifling clinicians’ ability to care for cancer patients.
She explains that SABR is often used for prostate cancer: “It’s not indicated for everybody, but for a selected group of patients who have very focused lesions, it’s useful and effective,” she says. “The difference between that and standard radiotherapy, which is still a great treatment, is that it can be one to five fractions of treatment—one to five visits for the patient—whereas standard radiotherapy can be up to six weeks or 30 visits.”
Reducing the number of treatments benefits both the patient and the healthcare system, Thorp states. “NHS England has acknowledged this, but to have the technique approved and commissioned is taking many, many months. SABR is still being treated as a ‘not-business-as-usual’ specialised technique, yet clinicians have been trained, and protocols have been written.” Although rigorous checks are necessary, she adds that “it often feels like we are hitting our heads against a brick wall”.
“Gross inequality” in cutting-edge treatments
In Peddu’s view, “gross inequality” in service distribution must be addressed by the NHS’s 10-year plan. He describes that there are no basic interventional oncology (IO) services across the south of England, meaning patients who are counties away must travel to King’s—Peddu’s centre—to gain access to any “quality IO”, including straightforward treatments such as bile duct decompressions for pancreatic or bile duct cancers or radioembolization treatments for primary liver tumours.
Access to the newest treatment is not universal, he emphasises. Peddu gives the example of selective internal radiation therapy (SIRT), a treatment now recommended by the National Institute for Health and Care Excellence (NICE) for primary liver tumours, which is only available in select centres across the UK.
“Centres that offer SIRT has just about reached double digits, whereas this must be at least three or four times more for the treatment to be universally rolled out and equitably distributed across the country,” says Peddu. This has not yet been achieved, which Peddu attributes to infrastructure and workforce shortages across the UK— two areas he hopes will be addressed in the upcoming NHS plan.
“What we’ve got now is a postcode lottery, which is completely against the principles of the NHS,” says Thorp. She details that the plan must reprioritise the clinician voice and place less focus on “complicated processes”. During the COVID-19 pandemic, she explains that processes were “swept away—the clinician’s voice was heard, and we were able to innovate to make very rapid progress”.
Thorp states that, although a degree of discernment is necessary, restricting all decisions by way of complex red tape is restricting the NHS’s potential to lead the way in innovation. “The NHS has a history of leading the world in amazing medical advances, such as transplant and dialysis, but now we risk being left behind,” continues Thorp.
Multidisciplinary team meeting reform
Elsewhere in the NHS plan, Thorp and Peddu both hope to see the multidisciplinary nature of modern cancer care addressed, with focus on reform of multidisciplinary team (MDT) meetings for more efficient diagnoses. In Peddu’s view, IO should have a central role here, as, in the early stages of diagnosis, IO is able to offer curative treatments.
“One of the ambitions of the cancer plan is to diagnose 75% of cancers at the T1 and T2 stage—very early stages—by 2028. You want to pick up the cancers early by establishing emphasis on diagnosis, but there should also be emphasis on deciding, when you pick up these cancers early, what is the most cost-effective way of treating these cancers—and this is where IO comes in,” says Peddu.
To Thorp, collaboration between all healthcare professionals and the opportunity to share ideas to make decisions around individual patient options is “absolutely key” to high-quality care. “This should not be revised,” she states. Rather, she believes more clearly defined “streamlined” MDT meetings could improve productivity and speed up diagnoses.
Thorp shares that a joint survey between Thiscovery and the RCR was recently sent to all staff who attend MDT meetings, to which they received 1,455 responses. They found that respondents reported the value of MDT working as well as MDT meetings, but inefficiency was frequently flagged as an issue concerning the latter.
“We are spending more and more time in MDT meetings,” Thorp says. “When they were initially developed, it was the view that every patient must be discussed to prevent one doctor from determining the care pathway with no oversight and therefore introducing variation in care. Now unfortunately, there is still a lot of unwarranted variation even with MDT meetings.”
Thorp states that a “lighter degree of scrutiny” is needed to seize the potential of MDT meetings as a vehicle for collaboration and a platform for the patient voice. Currently, clinicians must discuss patient cases in MDT meetings before initiating treatment, which can slow down diagnoses if the meeting occurs once weekly, Thorp explains.
She continues: “We’re not looking to stop MDT meetings. They have great potential to improve standards for care, but we need to reassess what they’re for. Are they just a forum to discuss lots of patients? We’ve gone a little too far down the path of dependence on MDT-backed decision making. Clinicians need to be confident that we won’t be criticised or taken to court if a patient wasn’t discussed in the MDT. This reassurance must come from the Royal Colleges, NHS England and the Department of Health and Social Care.”
“Once-in-a-decade opportunity”
Expected in early 2026, Peddu hopes that the NHS 10-year plan for cancer care will take “all of these factors into consideration and ensure that there’s seamless delivery of the service without super-rounded bureaucracy or multiple ring-fencing of everything”.
Conversely, if the plan continues to propose change without consideration of limiting processes, he believes that “suboptimal delivery” of cancer care will lead to poorer outcomes for patients. “It’s a once-in-a-decade opportunity,” Peddu concludes, as he and others now await the release of the national cancer strategy in the coming months.