The ASTER randomised clinical trial that examined the effect of endovascular contact aspiration vs. stent retriever on revascularisation in patients with acute ischaemic stroke and large vessel occlusion in the anterior circulation found that first-line thrombectomy with contact aspiration compared with stent retriever did not result in an increased successful revascularisation rate at the end of the procedure.
As Bertrand Lapergue (Department of Stroke Center and Diagnostic and Interventional Neuroradiology, University of Versailles and Saint Quentin en Yvelines, Foch Hospital, Suresnes, France) and colleagues reported in JAMA in August, the benefits of endovascular revascularisation using the contact aspiration technique vs. the stent retriever technique in patients with acute ischaemic stroke remain uncertain because of lack of evidence from randomised trials.
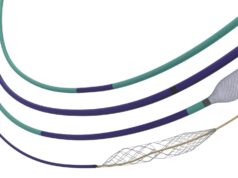
The ASTER (Contact aspiration vs. stent retriever for successful revascularization) study was a randomised, open-label, blinded endpoint clinical trial conducted in eight comprehensive stroke centres in France (October 2015–October 2016). According to the investigators, patients who presented with acute ischaemic stroke and a large vessel occlusion in the anterior circulation within six hours of symptom onset were included.
The triallists randomised 381 patients (mean age, 69.9 years; nearly 46% women) to either receive first-line contact aspiration (n=192) or first-line stent retriever (n=189) immediately prior to mechanical thrombectomy.
As summarised in the JAMA article, the primary outcome was the proportion of patients with successful revascularisation defined as a modified Thrombolysis in Cerebral Infarction (TICI) score of 2b or 3 at the end of all endovascular procedures. The secondary outcomes included degree of disability assessed by overall distribution of the modified Rankin Scale (mRS) score at 90 days, change in National Institutes of Health Stroke Scale (NIHSS) score at 24 hours, all-cause mortality at 90 days, and procedure-related serious adverse events.
Results
Trial results revealed that 363 completed the trial. The median time from symptom onset to arterial puncture was 227 minutes. For the primary outcome, the proportion of patients with successful revascularisation was 85.4% in the contact aspiration group vs. 83.1% in the stent retriever group p=0.53. For the clinical efficacy outcomes (change in NIHSS score at 24 hours, mRS score at 90 days) and adverse events, there were no significant differences between groups.
Penumbra provided an institutional grant to support the ASTER trial.