Prostate artery embolization maintains its effectiveness for at least three years after patients undergo the therapy, according to research presented at the Society of Interventional Radiology’s 2017 annual scientific meeting. The study was awarded as the “Abstract of the Year”.
This study of 1,000 men is the largest of its kind to evaluate the long-term effectiveness of prostate artery embolization.
Researchers also found that embolization is especially effective in men with benign prostatic hyperplasia who also have acute urinary retention or the inability to voluntarily urinate and in patients with very large prostates who are normally treated with open surgery.
“Prostate artery embolization gives men with benign prostatic hyperplasia a treatment option that is less invasive than other therapies and allows them to return to their normal lives sooner,” said João Martins Pisco, an interventional radiologist at St Louis Hospital in Lisbon, Portugal, and the study’s lead author. “Time and time again, I see patients who are relieved to find out about prostate artery embolization because they are not able to tolerate medications for benign prostatic hyperplasia due to their side-effects. These men also do not want traditional surgery because it involves greater risks, has possible sexual side-effects, and has a recovery time that is relatively long compared to prostate artery embolization, which is generally performed under local anaesthesia and on an outpatient basis.”
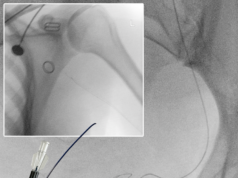
Between March 2007 and March 2016, Pisco and his team performed prostate artery embolization on 1,000 men with the average age of 67 years. All patients were evaluated in the short term (one, three, and six months); 807 patients were seen through the medium term (every six months between six months and three years), and 406 patients were evaluated long term (every year after three years).
During each evaluation, the men’s symptoms were measured by the International Prostate Symptom Score (IPSS), which tests for the blockage of urine flow, and the International Index of Erectile Function (IIEF), which assesses erectile dysfunction. Researchers also measured the size of the prostate and the amount of urine left in the bladder after urination. They also evaluated the peak urinary flow rate and the prostate-specific antigen (PSA) level, a test used to screen for prostate cancer.
The data from these measures revealed at the short-term mark that the treatment had an 89% cumulative success rate—measuring the success across all variables through the given testing period.
The 807 men evaluated at the medium-term mark had an 82% success rate. And of the 406 patients measured at the long-term mark, 78% were considered cumulative successes.
“Our results demonstrate that this minimally invasive treatment is successful in the long term and should always be presented to patients who are exploring options to resolve their benign prostatic hyperplasia,” remarked Pisco.
In an additional analysis, researchers found that among 112 patients who also suffered acute urinary retention before undergoing embolization, 106 or 94.6% had their catheter removed between two days and three months after treatment. At medium-term and long-term follow-up, 95 of the 112 (84.8%) and 89 of the 112 (78.5%) did not experience any recurrence of their acute urinary retention.
The team also performed prostate artery embolization in 210 patients who had limited treatment options due to extreme enlargement of the prostate (larger than 100cm³). Of these men, 84% experienced cumulative success at short-term evaluation and 76.2% at medium- and long-term. The normal size of a prostate is 15–30cm3.
While this research demonstrated that prostate artery embolization was highly successful, Pisco noted that the treatment may not be appropriate for all patients, such as those with advanced arterial atherosclerosis that may be due to smoking or diabetes.
As a next step, researchers are now conducting a study comparing the effectiveness of prostate artery embolization to a sham—or placebo—treatment to address any possible placebo effect that may have occurred during Pisco’s research with these 1,000 patients.