At CIRSE, Derrick Martin, University Hospital of South Manchester NHS Foundation Trust, Manchester, UK, discussed different approaches, including interventional procedures, to managing pancreatic necrosis—stating that one of the key principles of management was to “wait as long as you can to intervene and then do as little as possible when you do intervene”
“About 20% of patients with acute pancreatitis will fall into the necrotising and severe category”, Martin told delegates. He added: “It is important to recognise that there are two phases to the illness. In the first phase, the patient is acutely unwell because of the reaction to the acute inflammatory process. These are the patients who die of multiple organ failure on the intensive care unit in the first week or so. Treatment for these patients is aimed at supportive therapy for their acute pancreatitis. Once we have got them over that phase, we enter into the second phase of necrotising pancreatitis, which is when we start to deal with the problems caused by the necrosis and the thing that kills these patients is infection.”
Prior to this second phase, Martin explained, the degree of necrosis should be determined using CT as the “extent of the illness and the extent of mortality generally goes along with the extent of the necrosis. CT done after 72 hours, that is four or five days after admission, will give you an accurate assessment of intra-pancreatic and extra-pancreatic necrosis.” Complications of pancreatitis include pseudocyst and Walled-off necrosis. However, it is important to distinguish between a pseudocyst, which is the result of acute peripancreatic fluid collection, and walled off necrosis. A pseudocyst, Martin said, does not contain solid material, rarely becomes infected, and resolves spontaneously (although some pseudocysts, mostly because of their size, will need to be treated).
Even if imaging does indicate the patient has walled off necrosis, intervention may not be necessary. Martin said: “Many of these collections, if they remain sterile, will slowly reabsorb the solid material and will liquefy. Over time, they will disappear.” The most obvious indication for drainage, he added, is infection because “this massively increases the risk of death.” He explained: “CT will readily demonstrate gas within a necrotic collection and probably indicate the presence of infection. But, just be aware that, uncommonly, these collections can spontaneously discharge themselves as they fistulate into the adjacent bowel and that might be the cause of the gas within the collection. The key is the size of the collection, which will spontaneously diminish if it has fistulated and discharged itself—whereas if the collection remains the same size as on previous imaging and now contains gas, then that would indicate the presence of infection.” However, the lack of gas on a CT scan does not mean that there is no infection. “There is a group of patients, quite a common group of patients, who do not have gas in the walled off collection but are still unwell. Their laboratory parameters are abnormal and they still need to be kept on the intensive care unit. In these patients, you should clinically suspect that they might have infected necrosis and that it might be appropriate to drain the collection.”
Current management approaches
Martin outlined different management approaches, stating management could be done in two stages. He said: “You can make an immediate difference to the patient by putting a drain into the infected walled off necrosis and then come to back deal with the necrosis at second stage at a later date.” He added that, for some patients, an interventional drainage procedure would be all that was necessary to treat them, saying “Prolonged drainage can allow liquefaction of necrotic material and ultimate resolution of the walled off necrosis.” However, the success of the drainage depends on the volume of solid material within the necrosis and the timing of the procedure. According to Martin, solid material can block catheters and this can lead to a longer stay on the intensive care unit, more episodes of acute infection, and more episodes of multiple organ failure, which in turn can lead to more mortality.
In terms of surgical approaches, Martin said that “most would agree that laparotomy, through a transperitoneal approach, is no longer the first-line approach. But, percutaneous retroperitoneal dissection with the placement of drains with the resection of necrotic tissue is seen as a good approach. This approach can be repeated as necessary in order to deal with the further collections of pus and further removal of necrotic material.”
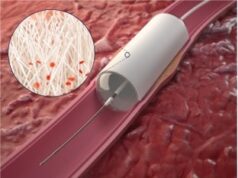
A combined approach to manage pancreatic necrosis, Martin explained, involving using a small drain to remove the pus and then steadily enlarging the drain, possibly under anaesthetic with a surgeon in attendance.
Future management approaches
The endoscopic approach, Martin stated, has been “well recognised” as an effective method of treating pseudocysts for some time. The procedure involves using endoscopic ultrasound to detect the collection, using a catheter to create a track, and placing various stents in order to provide drainage. He added that, previously, the procedure was “slightly more tricky” for managing pancreatic necrosis because of the size of the stents used. However, Martin explained, the situation is improving because “Endoscopists now use a balloon to dilate the transgastric tract into the walled off necrosis and pass the endoscope through the track, using snares and biopsy devices to remove the necrotic material.” He added that there was now a specifically designed stent which can be placed between the gastric wall and the walled off necrosis collection and the necrotic material can be drained. There is also a biodegradable stent designed for this indication. Endoscopists have always been fearful of the possibility that a stent will fall into the walled off necrosis and create its own problems.” According to Martin, the benefits of the endoscopic approach are “pretty obvious” and include no external drain, no abdominal pain, patients being easier to nurse, and patients being more mobile. He added: “Patients die in bed in hospital. If you get them out of bed, they have a better chance of survival.” However, he said that bleeding was complication and that it was it important to do a preliminary enhanced CT to detect pseudoaneurysms to make sure “you don’t get any nasty surprises when you start your drainage procedure.”
Summing up his talk, Martin said: “The principles here are to wait as long as you can to intervene and do as little as possible when you do intervene. From that standpoint, it seems to me that the endoscopic approach has a got great future waiting for it.”