
This article is sponsored by Guerbet.
Christof M Sommer, Thilo Hackert and Götz M Richter discuss the renaissance of Lipiodol-based lymphangiography following a decline in its use in lymphatic interventions at the start of the millennium. They cite this return to Lipiodol (Guerbet) as being directly connected to an increase in the number of patients suffering from lymphatic leakage caused by complex surgical procedures, labelling the contrast agent “indispensable” in a lymphatic interventions programme. The rise in Lipiodol usage is here to stay, they argue.
Introduction
The story of Lipiodol-based lymphangiography and lymphatic interventions starts in 1901, when the French pharmacist Marcel Guerbet synthesised Lipiodol, an iodinated poppy seed oil, today commercialised as Lipiodol Ultra Fluid. After the accidental discovery of lymphangiography during routine hystersalpingography by Charles Várady, an enormous amount of specific knowledge and skill accumulated. During the 20th century, Lipiodol-based lymphangiography was excessively used as a diagnostic procedure. Around the turn of the millennium, however, the numbers of patients undergoing lymphangiography decreased considerably, most likely since alternative noninvasive imaging modalities such as MRI became available. In the following years, interest in and competence to perform lymphangiography got lost in hospitals around the world. Interestingly, during the last decade, the pendulum swung back, and a high demand for diagnostic and therapeutic lymphangiography was noted. We believe that this phenomenon is directly connected to the increasing number of patients suffering from therapy-refractory lymphatic leakage caused by surgical procedures of great complexity. Today, Lipiodol is indispensable for all institutions with a lymphatic interventions programme.
Indications and outcomes
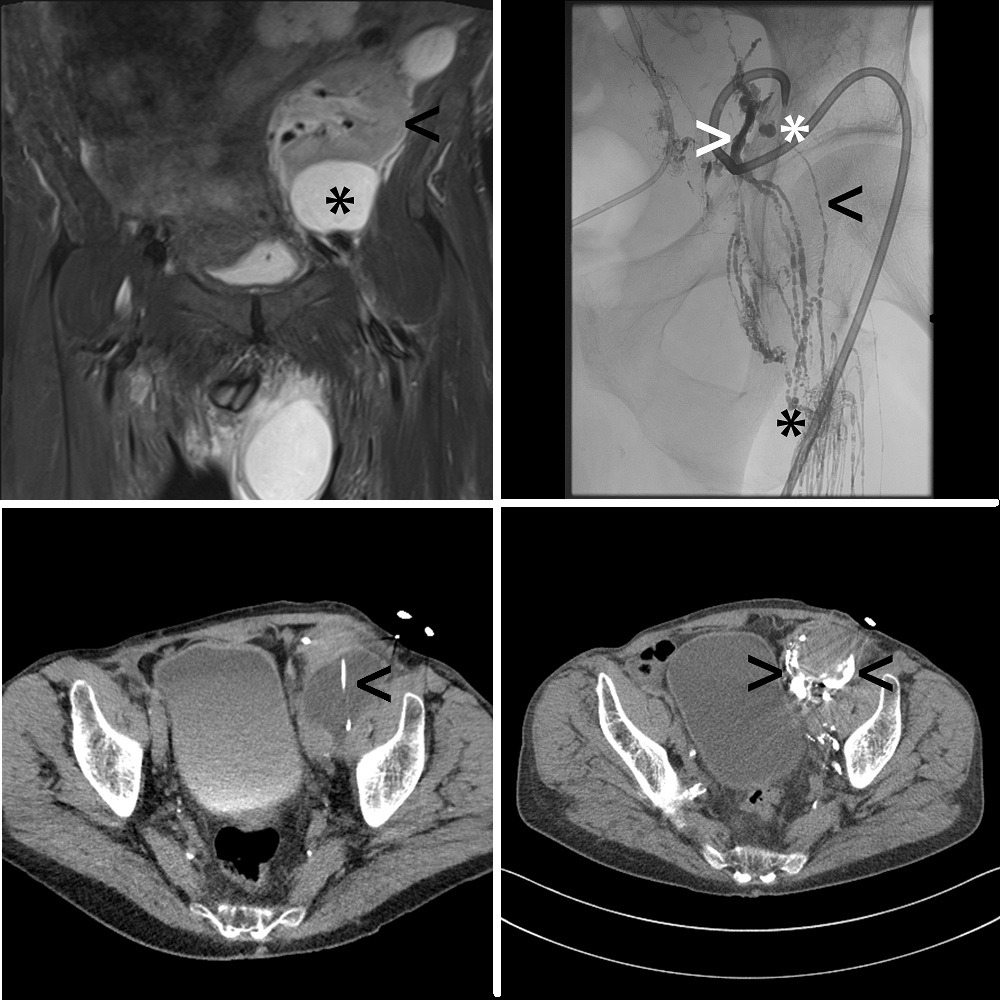
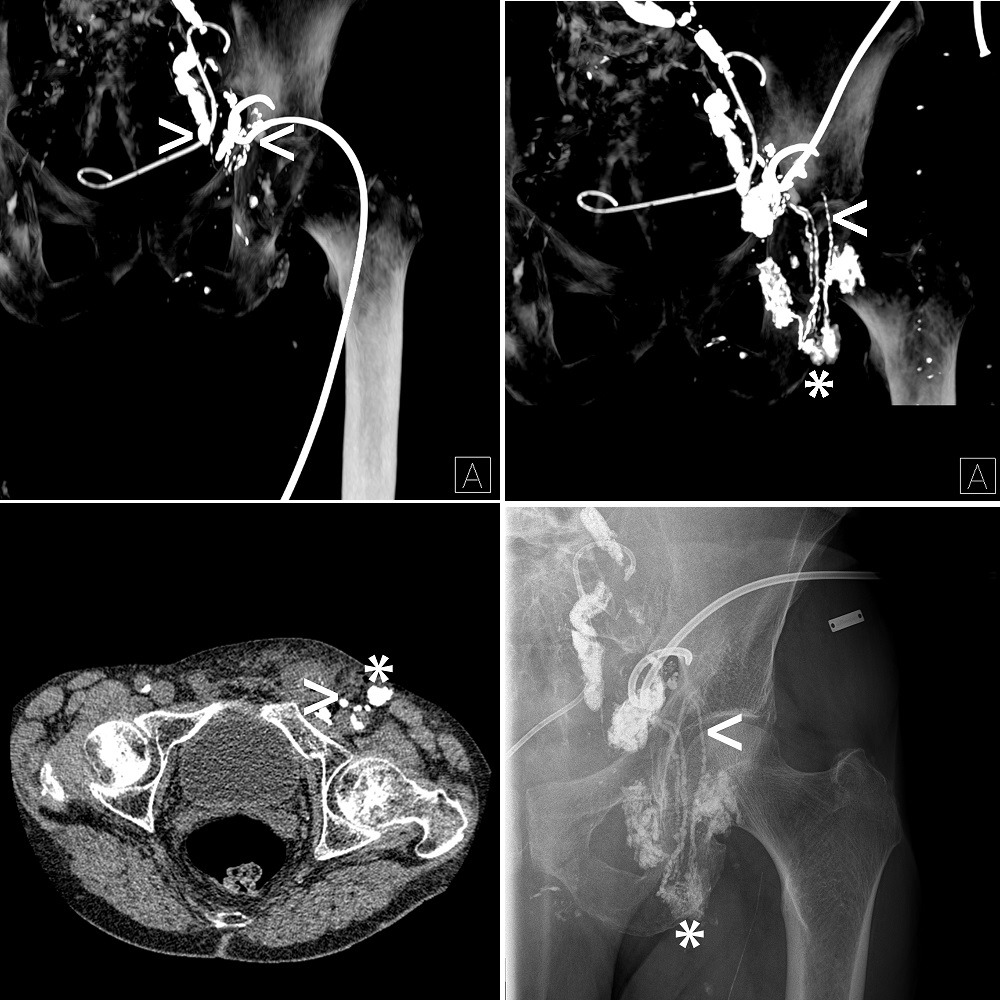
Lipiodol-based lymphangiography and lymphatic interventions can cure different types of highand low-output iatrogenic (for example, chylous ascites after ultra-radical lymphadenectomy) and spontaneous (for example, pulmonary lymphatic perfusion syndrome) lymphatic leakages. Typically, lymphangiography is performed either with the transpedal or intranodal application of Lipiodol under X-ray imaging, with the following outcome parameters: technical success rate of 90–100%, Lipiodol injection volume of 0.5–40ml, Lipiodol injection speed of 0.3–60ml/hour, complication rate of 0–22%, 30-day procedure-related morbidity and mortality rates of 0% and 0%, respectively, and clinical success rate of 51–100% for transpedal lymphangiography and 33–100% for intranodal lymphangiography (according to the literature published between January 2007 and May 2017, and for patients suffering from post-operative therapy-refractory lymphatic leakage). Second-line lymphatic interventions, feasible on the same day as, or a few days after, Lipiodol-based lymphangiography, include many different procedures, such as interstitial embolization or thoracic duct embolization. Outcome parameters include technical success rate of 89–100% for interstitial embolization and 50–100% for thoracic duct embolization, Lipiodol/cyanoacrylatebased medical glue injection volume of 0.5–8ml, Lipiodol/cyanoacrylate-based medical glue mixing ratio of 1:2–20:1, complication rate of 0–22%, 30-day morbidity and mortality rates of 2% and 0%, respectively, and clinical success rate of 80–100% for interstitial embolization and 90–100% for thoracic duct embolization.
Conclusions
Lipiodol plays a key role in lymphangiography and lymphatic interventions. For patients with iatrogenic and spontaneous lymphatic leakage, Lipiodol is the only pharmaceutical drug approved for radiological imaging of the lymphatic system. Following the application of Lipiodol, fluoroscopy, radiography and, in particular, computed tomography enable the precise visualisation of the different types of lymphatic leakages. Looking at published data, in conjunction with our long-standing experience at Stuttgart and Heidelberg—more than 600 transpedal lymphangiographies performed over the last three decades—it becomes evident that Lipiodol unquestionably features not only important diagnostic, but also therapeutic, characteristics. Selective and persistent blockage of the diseased lymphatic vessels and sterile inflammation reactions with subsequent tissue scarring result regularly in the cure of lymphatic leakage. Lipiodol is also mandatory for second-line lymphatic interventions. Doxycycline- or ethanol-based sclerotherapy and EVOH (ethylene vinyl alcohol)-based liquid embolization show non-satisfying outcomes, especially in the setting of high-output lymphatic leakage, and therefore cyanoacrylate-based medical glue is regularly used instead. Not only for X-ray visualisation issues, but also for the specific adjustment of glue polymerisation time, Lipidodol is mixed with cyanoacrylate-based medical glue in different ratios.
Future directions
Lipiodol-based lymphangiography can be performed as a highly standardised and safe diagnostic and therapeutic radiological treatment. Second-line lymphatic interventions are associated with a higher degree of technical failure, complications, and morbidity, but also with a higher degree of clinical success. Currently, lymphangiography and lymphatic interventions are performed only in specialised centres, and not as nationwide primary care. This is the result of limited theoretical and practical knowledge in the radiological and referring community. Optimised radiological strategies, together with interdisciplinary consensus, should be published in the form of guidelines with the intention of promoting the best lymphatic care. The first steps towards achieving the strong evidence base have already been taken, with a prospective, randomised controlled multicentre trial currently being performed in South Korea, comparing interstitial embolization using Lipiodol and cyanoacrylate-based medical glue versus sclerotherapy in the management of symptomatic postoperative pelvic lymphocele. Nevertheless, the optimal pharmaceutical drug for second-line lymphatic interventions has not been developed yet. There have been speculations as to whether different versions of Lipiodol with even higher viscosity or a Lipiodol containing non-adhesive precipitating liquid embolic could further increase safety and efficacy. We have witnessed the successful renaissance of Lipiodol in lymphangiography; however, the reincarnation of Lipiodol in second-line lymphatic interventions is still an important objective. In the future, the number of patients with lymphatic leakage undergoing radiological treatment will dramatically increase, as soon as different problems (such as communication barriers between medical disciplines and the under-reporting of candidates) are solved.
Christof M Sommer is an interventional radiologist at the Clinic of Diagnostic and Interventional Radiology and 1st Siemens European Reference Site for Interventional Oncology and Radiology, Klinikum Stuttgart, Stuttgart, Germany, as well as an assistant professor of radiology at the Clinic of Diagnostic and Interventional Radiology, Heidelberg University Hospital, Heidelberg, Germany. He has received a speaker honourary from Guerbet.
Thilo Hackert is a professor at and deputy head of the Department of General, Abdominal and Transplantation Surgery, Heidelberg University Hospital and section chief at the European Pancreas Center, Heidelberg University Hospital, Heidelberg, Germany. He has no conflict of interest to report.
Götz M Richter is a professor at and medical director of the Clinic of Diagnostic and Interventional Radiology and 1st Siemens European Reference Site for Interventional Oncology and Radiology, Klinikum Stuttgart, Germany. He has no conflict of interests to report.













