The results of an American College of Radiology (ACR) survey find that small hospitals and rural communities experience greater difficulty recruiting and retaining interventional radiologists (IRs) and meeting IR service demands compared with their non-rural counterparts. The data were published recently in the Journal of the American College of Radiology in an article authored by Eric Friedberg (Department of Radiology and Imaging Sciences, Emory University School of Medicine, Atlanta, USA) and colleagues.
The study investigators worry that these data evidence a “potential subspecialist manpower crisis”, with geographic factors playing an important role in determining patient access to IR services. Upon evaluating the survey results, the authors conclude the “data suggest that small and rural hospitals will be disproportionally affected by future predicted physician shortages, resulting in difficulty meeting both general and subspecialty radiology service needs”.
Friedberg and colleagues sought to capture information regarding the current status of IR staffing across the USA, and to evaluate the perspectives of radiologists across the nation regarding their ability to recruit and retain interventionalists. Via email, they sent out a 22-question survey—finalised by an ACR intercommission workgroup comprised of members from the Commissions on General, Small, Emergency, and/or Rural Practice and the Commission on Interventional and Cardiovascular Radiology—to 15,463 ACR members who self-identified in the ACR Practice of Radiology Environment Database as a “group practice leader,” “general radiologist,” “interventional radiologist,” or “abdominal radiologist.” However, the response rate was low; the conclusions are based on the answers given by the 1,005 email recipients who completed the survey.
Rural radiology practices have more difficulty meeting local demand for IR services
Compared with non-rural equivalents, the study finds that rural radiology units experience more difficulty meeting local demand for IR services, both at the hospital level and the regional hospital catchment area.
A statistically significant greater proportion of responders from rural hospitals compared with non-rural hospitals, the latter defined as those serving an estimated population of 250,000 or more, answered that their group falls far short of the demand for IR services: 6% of rural answers, compared to just 0.9% of non-rural ones. A further 23.1% of rural responders believed that the hospital they work at falls short of the demand for IR services. In comparison, only 13.4% of non-rural IRs thought this about their workplace.
In addition, a greater proportion of non-rural IRs said that their group meets the demand for IR services: 48.2% of rural responders, compared to 60.8% of non-rural survey participants.
The authors also note the relevance of having an exclusivity clause in IRs’ contracts. A greater proportion of responders from both rural and non-rural hospitals where they were able to meet most requests for IR procedures indicated that they did have an exclusivity clause in their contract. In comparison, in hospitals where there was a desire for IR procedures that could not be delivered, i.e. where local demand for IR services was not being met, a greater proportion of responders from both rural and non-rural areas did not have an exclusivity clause in their contract.
In addition, when respondents believed catchment area demands were being met, they more often responded that the IR physicians in their group do not take diagnostic radiology call. Similarly, physicians who reported not meeting IR needs more often reported having primary diagnostic responsibilities.
Rural radiology practices experience more difficulty recruiting IRs
More survey respondents from rural areas had trouble recruiting IR physicians to their practice than non-rural workers did; 59.2% of rural IRs reported this difficulty, compared to 32.8% of non-rural answerers. According to Friedberg et al, “Of rural respondents who perceived they had difficulty recruiting IR physicians to their practice, 58.7% believed that ‘IR physicians do not want to do diagnostic work’ was a factor, which cumulatively accounted for 24% (20.0%, 28.6%) of all responses. Of rural respondents who perceived they had difficulty recruiting IR physicians to their practice, 58.2% believed ‘IR physicians do not want to work in a small or rural setting’ was a factor, which accounted for 29.8% (19.8%, 28.4%) of all responses. Together, these two reasons accounted for 47.8% of all rural respondents’ answers.”
It is harder for rural radiology practices to retain IRs
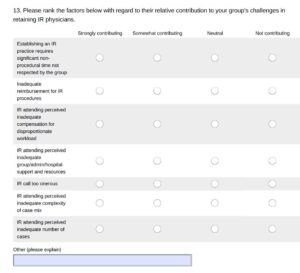
Over 38% of respondents from rural hospitals reported difficulties with retaining IR physicians in their practice, as opposed to 23.5% of non-rural IRs experiencing the same issues. “IR attending perceived inadequate complexity of case mix” was the largest explanatory factor listed among rural responders, with 67.5% listing this as the top reason for the low retention rate. As expected by the study investigators, fewer non-rural responders, who nevertheless also thought they had difficulty retaining IRs in their own teams, cited this as an issue, with just over half citing inadequate case mix complexity as the number one source of low IR retention in their practice.
The number of available cases was also seen as a contributing factor to a reduced ability to retain IRs for rural responders, but not so much amongst non-rural answers. Two-thirds of rural responders believed an inadequate number of cases to be a contributing factor, whereas fewer than one-third of non-rural responders did. Cementing this difference, 18.1% of non-rural answers claimed that an inadequate number of IR cases was not a contributing factor at all.
The study authors hypothesise: “The overall subjective trend in responses may reflect an underlying desire by IRs to exclusively practice “high end” IR—a trend that may be exacerbated as a large of integrated pathway graduates soon begin entering the workforce”.
New integrated training pathways approved
The American Board of Medical Specialties has recently approved new integrated training pathways for IRs. There are now 78 integrated IR residency programmes currently accredited by the US Accreditation Council for Graduate Medical Education (ACGME), which Friedberg et al describe as “supplanting traditional diagnostic radiology residencies for those who seek highly specialised IR practices”.
However—despite the aim of increasing subspecialisation being to foster a more focused discipline with a greater commitment to longitudinal clinical care—thought leaders have expressed the fear that introducing more niches may exacerbate evolving patient access issues. Friedberg and colleagues write: “Specifically, questions remain around whether this trend will increase the risk that small and rural hospitals will have difficulty recruiting and retaining IRs who no longer seek to provide diagnostic radiology services, potentially leading to hospital administration, referrer, or patient dissatisfaction—as well as endangerment of future radiology contractual relationships”.
The authors go on to comment: “The inability to provide adequate IR services may be a contributor to hospital and referrer dissatisfaction, as well as to patient care underperformance in rural and small areas—a situation that is likely to worsen amidst superimposed training pathway changes, healthcare system consolidations, and projected physician shortages. Respondents to this specific survey consistently indicated that IR services stabilise groups and add value beyond revenue.
They conclude: “Given the value of IR services to patients and the ongoing geographic access challenges to those services as the practice of IR services becomes increasingly subspecialised, professional societies, such as the ACR and the Society of Interventional Radiology, are likely to play a critical role in developing plans and solutions to guide radiology practices. Potential solutions include managing expectations for new pathway trainees, development of additional training opportunities for general radiologists to provide a broader range of at least less complex interventional procedures, novel contractual and practice organisational options for IRs, illumination of the ‘downstream revenue’ value in IR, and synergistic partnering or alliance with other subspecialties or larger institutions”.










