“Interventional radiologists should not be cavalier about protecting ideas, but focusing on maximising rewards has sidelined more ideas than it has helped individual inventors. Sadly, in many cases innovation and entrepreneurship have become interchangeable; rather than focusing on solving a problem, the thoughts turn immediately to how to maximise monetary return,” says Lindsay Machan, an indefatigable innovator with nearly 140 patents to his name, who is perhaps most widely known for his contribution to developing and commercialising the paclitaxel-coated stent. Machan is an interventional radiologist at the Vancouver Hospital and an associate professor of Radiology, University of British Columbia, Vancouver, Canada.
What drew you to medicine and interventional radiology?
Right up to the time I attended university, I wanted to be a lawyer. Then I actually met one. I was looking for a career where on most days, I could feel good about what I had done, that I had contributed in some way. Medicine and in particular interventional radiology have been a perfect fit for me. I was exposed to interventional radiology during my residency because Joachim Burhenne, one of the pioneers in biliary interventions, was our department chairman. I loved the need to improvise during procedures and the immediacy of the discipline.
Who were your mentors and what did you learn from them?
I likely would have quit interventional radiology early on if I had not worked with Dr Rebecca Peterson in Ottawa during my interventional fellowship. She was extremely encouraging, patient, and had magical catheter skills. My first consultant job was at the Hammersmith Hospital in London with Professor David Allison and (now Professor) Andy Adam. From them, I learned to assess procedure outcomes without preconceived ideas of efficacy and to incorporate a clinical focus. My first project in London was an assessment of balloon dilation of the prostate; we found that when objective criteria were applied, the procedure did not work. I also learned that disproving a procedure initiated by one’s ex-boss may not be the wisest move politically. My next position was at the University of Pennsylvania with Stan Cope [Constantin Cope]. Stan’s overriding principles were to do procedures and innovations that are relevant to patient care: he felt if a procedure we offer is not better than other ways to treat a given condition, we should not do or promote it. So the overriding principle was to ensure that the patient gets the best care, not a procedure just because it is one done by our specialty. In innovation his mantra was “keep it simple, stupid”; the latter part often (appropriately) directed at me.
You have an abiding interest in innovation after, legend has it, witnessing Dr Joachim Burhenne in Vancouver performing the first-in-man balloon dilation of the prostate on himself. In your view, what can interventional radiology, a specialty that defines itself by its innovation, do in order to foster and promote innovation?
I do not think that innovation can be taught. Innovators have an innate need to improve things. Interventional radiology attracts people who are attracted to problem-solving, so we are always going to be an innovative specialty because we have the most important ingredient—bright, energetic minds. Sadly, in my opinion, in many cases innovation and entrepreneurship have become interchangeable; rather than focus on solving a problem, the thoughts turn immediately to how to maximise monetary return. That is not to say that interventional radiologists should be cavalier about protecting ideas, but focusing on maximising rewards has sidelined more ideas than it has helped individual inventors. In particular, interventional radiologists are blessed to be able to work with companies whose very lifeblood has been innovation. Although working early with companies will not result in the highest monetary returns or control of the process, these companies understand the process, have amazing expertise, and ideas with merit will generally find their way into clinical use, which at the end of the day is the key aspect of innovation in medical care. For most busy physicians with a good idea, approaching one of these companies will be a more practical route to actually seeing their idea reduced to practice. The major barrier to innovation I see is the degree of oversight by risk averse administrators (including physician administrators) that make any perceived non-optimal outcome as a reason for blame.
You have been issued around 140 patents including the one for anti-angiogenic compositions and methods of use (patent describing paclitaxel stent coating). In your view what are the most interesting innovations currently on the horizon, but not yet in clinical practice?
In the current regulatory and financial climate I believe that the area of “big data”, the application of now-ubiquitous uber-powerful computing to every conceivable dataset will have the most profound impact on our day to day practice. Near-term applications in this area include online decision support and appropriateness criteria, extraction of additional data from commonly used exams like electrocardiograms or CT angiographies and billing. Intermediate-term applications include interfacing with personalised genomics to optimise therapy and automated image reading, including real-time reading of imaging such as ultrasound. Other areas I find interesting are biologically active devices, including resorbable stents and personalised genetics, however, cost and regulatory burden mean that incorporation into practice may not be as fast as we have seen in the past.
Also, seeing as prostatic artery embolization is such a hot topic right now, could you tell us more about the patent you have been issued for “system for treating benign prostatic hyperplasia”?
It is a device for simple transurethral irreversible electroporation. It most likely would not be used in the same patient group who are most appropriate for prostatic artery embolization.
As a co-patenter of the paclitaxel stent, licensed to Cook and Boston Scientific, how did the idea for developing this device came about?
I had been exposed to the earliest clinical use of the stent while working in the UK and became aware of the issue of restenosis, which at that time was a little-used term. A few unsuccessful ideas, mainly around radiation and heating, ensued. After returning to the University of British Columbia, we set up a weekly teaching rounds with vascular surgery alternating presentation each week. A vascular surgeon was thankfully too disorganised to prepare rounds one week, thrusting a medical student in to give a lecture on his pre-med research in cartilage derived extracts on animal models of rheumatoid arthritis. During this round, I accidentally stirred to attention. At the end of the talk I told the presenter I knew nothing about rheumatoid arthritis but this would be a fantastic stent coating. To which my eventual partner on this project replied: “what is a stent?” We became co-founders of Angiotech Pharmaceuticals which started out with the idea of angiogenesis inhibition, but which eventually lead to the paclitaxel-coated stent which was licensed to Cook and Boston Scientific. In 2006, Dr Bill Hunter and I shared the Manning Foundation Innovation Award for developing and commercialising the paclitaxel-coated stent.
As one of the founders of Ikomed Technologies, a company that seeks to reduce radiation from fluoroscopic medical imaging procedures using a proprietary actuator technology and image processing, can you tell us more about the technology and how it works?
It is a dynamic collimation system that can potentially reduce the radiation exposure of a procedure up to five-fold without image degradation. It consists of a rapidly moving lead shutter (which works in addition to the existing manual collimation system), placed between the X-ray source and the patient, and image-blending software. During fluoroscopic procedures, even with excellent coning, the physician is typically focused on a small portion of the image, usually where there is movement of a device. The remainder of the screen image provides context. The system allows different radiation doses to different parts of the image, with the highest in the region of interest. So a “normal” fluoro pulse rate (eg 15 fps) is chosen by the operator for the predetermined area of active interest. At a slower rate (eg once per second), the cones open to the full area chosen by the operator and then return to the more rapid tighter coning. All acquired images are blended in real-time, thus the projected image looks like normal fluoroscopy. The reduction in radiation dose depends on the size and frame rate of the active coning area, which is chosen by the physician. There is also a version where the area of active coning is altered in position and size by automated software that tracks catheter movement or contrast injection.
As one of the founders of the Canadian Interventional Radiology Association (CIRA) in 2001, can you describe what the next key steps for interventional radiology in Canada should be?
We are blessed with a really strong group of interventional radiologists across our country, particularly the younger generation, so talent is not our issue. Canada is one of only two countries where private medicine is illegal, so everyone works in the public system. The system is funded in precisely the same way as the Soviet farming and industrial collectives of the 1960s; senior bureaucrats foretell the amount of disease that will occur in the following year and at what cost it will be treated. This is not an optimal system to introduce innovation. Within this system, the most vital task for interventional radiologists is the gathering of data to prove the vital role of interventional radiology and for CIRA to promote this data to ensure interventional procedures are properly funded.
As coauthor with Kris Kandarpa of the Handbook of Interventional Procedures (the largest selling interventional textbook worldwide), what is the most important message on interventional radiology education that you would like spread?
Our specialty does an excellent job teaching the mechanics of procedures, we are not as good at teaching clinical judgement and how diligence in clinical care and close working relationships with our clinical colleagues are as important in practice development as technical competence.
What are your current views on angioplasty and/or stenting to alleviate symptoms of chronic cerebrospinal venous insufficiency? At what point is the sham trial that you are involved in running?
We continue to believe that although the intense media interest has decreased, it is important for multiple sclerosis patients and endovascular procedures in general that a blinded, controlled study be performed. From University of British Columbia we are leading a multicentre, Canadian, blinded trial on balloon angioplasty in patients with multiple sclerosis. Patients receive both a sham procedure and angioplasty during the trial. The trial will be completed July 2016. We remain fully blinded to the results.
Please describe a memorable case that you treated and why you remember it.
Two cases come to mind. One was a couple who emigrated to Canada, being told by a well meaning doctor in their native country that the wife should lie with her buttocks elevated on a pillow for two hours after mid-cycle intercourse in order to conceive a child. They followed this advice faithfully for 12 years. About a year after a 15-minute skin to skin varicocoele embolization, I was in a shopping centre when I ran into the couple with their newborn. The husband was so happy he was crying. I nearly joined him. The second case is that of 17-year-old girl with a traumatic aortic tear and intracranial haemorrhage, precluding any heparisation. A Hail Mary was called for. This was before commercial thoracic stent grafts, so I hand peeled and sewed a polytetra flurothylene graft onto bare Z stents and delivered it through a modified non-haemostatic homemade sheath. Two years later she and her mother stopped by to tell me she was enrolling in university and she has gone on to a career in healthcare. We tend to focus on and are proud of the technical and imaging aspects of our procedures, but both these cases brought home that what we do has an intensely human side and we can profoundly impact lives.
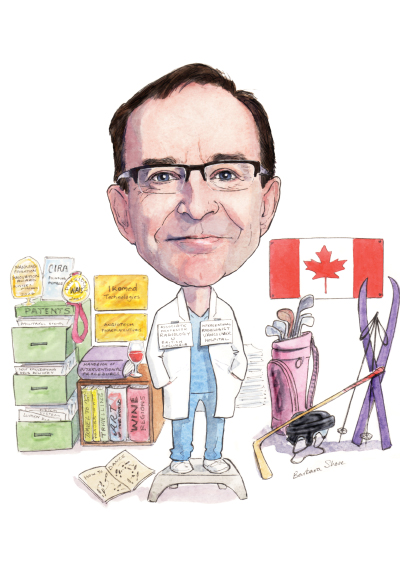
What are your interests outside of medicine?
Besides being fascinated by medical devices and medicine, I enjoy (and display exuberant incompetence at) golf, ice hockey, cross country and downhill skiing, and running. I read daily and am also interested in travel, art, and wine. I wish I had better hair and knew how to dance.
Fact file
Current position
1989– Interventional radiologist, University of present British Columbia Hospital Vancouver, Canada. Established interventional radiology department from de novo. Associate professor of Radiology at the University of British Columbia
Previous position
1989 Visiting assistant professor, University of Pennsylvania, Pennsylvania, USA
1987–88 Locum consultant, Hammersmith Hospital, London, UK
1983–86 Resident, Radiology, University of British Columbia, Vancouver, Canada
First-in-man procedures
1988 Fluoroscopically-guided prostatic stent
1994 Removable metallic urethral stent
1996 Paclitaxel-coated stent
1999 Paclitaxel-coated vascular stent,
1999 Translumbar endoleak repair using Onyx (Medtronic), with Bart Dolmatch
2002 Biologically active venous valve, with Dusan Pavnik
Awards
2015 2015 SIR Foundation Leaders in Innovation Award
2011 CIRSE Distinguished Fellow
2008 International Symposium of Endovascular Therapeutics (ISET) Innovator Award
2006 Manning Foundation Innovation Award, principal award winner for developing and commercialising paclitaxel stent
Society positions
2001 President, Western Angiographic and Interventional Society
2001 Founding member, Canadian Interventional Radiology Association (CIRA)
2002–06 Executive member at large, CIRA
1990–92 Canadian counselor Pacific Northwest Radiologic Society
2007–14 Board Member, BC Science World
Innovation/commercialisation
1992 Co-founder Angiotech Pharmaceuticals Vancouver, Canada
2010 Co-founder Ikomed Technologies, Vancouver, Canada
– Over 700 lectures, 19 that are keynote or eponymous













