The interim results of a multicentre, European retrospective analysis investigating the use of drug-coated balloons (DCBs) in symptomatic central venous stenosis (CVS) suggest that these devices could be a valid option for treatment, slowing down the effect of neo-intimal hyperplasia (NIH) leading to restenosis. Though with data mining still underway, the investigators warn against drawing any premature conclusions. Panagiotis Kitrou (Patras University Hospital, Patras, Greece) presented these preliminary results at the annual EndoVascular Access Meeting (EVA; 21–22 June, Patras, Greece) earlier this year.
Against the backdrop of the current paclitaxel controversy (where Konstantinos Katsanos, along with Kitrou and other colleagues, reported in the Journal of the American Heart Association (JAHA) an increased risk of death at two and five years following the use of paclitaxel devices), Kitrou first provided insight into how the publication has affected his own clinical practice. He told delegates: “We [at Patras University Hospital] have not changed our practice with regard to DCB use in dialysis access management. We believe that paclitaxel is an independent predictor of death, but its effect is different in different populations. Thus, a claudicant suffering more comorbidities compared to a claudicant with fewer comorbidities will have a greater number of factors antagonistic for the same event, which is death. Hence the signal and the effect of paclitaxel becomes faint and diluted while the actual benefit from NIH inhibition becomes more apparent.”
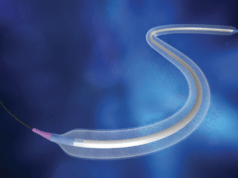
For patients with CVS, the gold standard treatment is percutaneous transluminal angioplasty (PTA). “However, Kitrou explained, “the patency rates may be as low as 28.9% at six months. This rate doubles to 60% when you use a high pressure balloon. The main problem [when using balloons] remains elastic recoil. You may also use a stent or a covered stent, is the latter being a much more aggressive treatment”.
Going through today’s evidence on CVS treatment, Kitrou showed EVA attendees the results from a 2015 retrospective analysis by Alexander Massmann et al that compared standard balloon angioplasty with paclitaxel-coated balloon angioplasty for symptomatic central vein restenosis in patients with impaired native haemodialysis fistulas. The study investigators concluded that paclitaxel-coated balloon angioplasty yielded a statistically significant longer freedom from target lesion revascularisation compared to standard balloon angioplasty. Although, Kitrou noted, Massmann and colleagues did include axillary veins, so he thinks these results “are not strictly for central veins”.
He next talked the audience through his own randomised controlled trial from 2017, which included 40 patients with de novo, restenotic and occluded lesions. Twenty patients were treated with the Lutonix DCB (BD), and twenty were treated with a non-coated balloon. In this study, the primary end-point was a clinically-assessed intervention-free period. In this, Kitrou et al found a significant difference in favour of DCBs. Additionally, DCB angioplasty was numerically better in the longitudinal analysis compared to plain balloon angioplasty.
Despite the fact that these studies found a significant difference between treatment arms consistently in favour of paclitaxel-coated balloons, Kitrou highlighted that these results have been observed in fewer than 30 patients. The present, multicentre European retrospective analysis therefore will provide data detailing DCB use in a greater number of patients. The primary outcome measures are a clinically assessed intervention-free period of the treated segment at six months, a dialysis access circuit with no need for clinically driven target lesion repeat intervention for symptom recurrence (verified angiographically), and no procedure-related minor and major complications.
The study included 87 patients from 11 centres across Greece, Germany, France, Italy, Portugal, and the UK. Though still only early data, the interim analysis reveals that at six months, the target lesion primary patency was 52%, and the median target lesion primary patency was 280 days, meaning lesions remained open following intervention for an average of nine months. “The results are already much better compared with our randomised controlled trial”, Kitrou said, referring to his 2017 study.
The investigators also measured primary patency of the access circuit. This was 48% at six months, and the median time to reintervention was 257 days. The access circuit survival was approximately 70% at six months, Kitrou shared.
“There is a lot of work in progress, we are still mining data—we are looking at this huge Excel [document] with a lot of data in there, and we will soon have more to share with you”, Kitrou concluded. interim interim