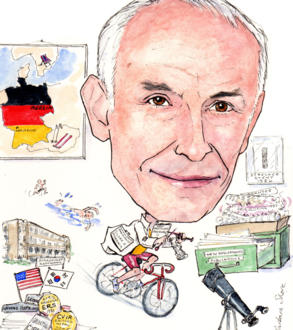
Professor Ernst-Peter Strecker invented his first bare-metal stent in around 1985. He was also one of the first to implant a stent in a patient with a post-PTA restenosis of the right common iliac artery, in May 1987. Later, he invented the first nitinol stent which is mainly used for malignant gastrointestinal strictures. He told Interventional News about all his passions — stents, science, sport and now stars!
It is an exciting time to be in interventional radiology, which has just been recognised as a medical specialty…
Yes! interventional radiology (IR) is a very interesting and exciting medical field. Interventional radiologists have completely developed many new procedures that have had a great impact on the treatment of many different disease entities. Interventional radiology represents minimally invasive medicine which becomes more and more required by our patients. It is especially important for palliative care and geriatric patients.
Further, it is cost effective combined with a relatively short hospitalisation. This is wanted by all our patients and also in general by our health systems.
It is crucial to note that interventional radiology does not depend on big machines. You just need a good fluoroscopy unit or angiographic machine to perform most of the Interventional radiology procedures. This is available in nearly all hospitals.
As an interventional radiologist you just have to buy a new device system which is usually not a big investment. There is no need to ask your hospital administration when you want to start using a new catheter for a new type of procedure in your angio lab, so we have a fair amount of freedom in our decisions to establish new procedures in our department. I feel that many other medical specialties are envious of our potential. Some of the procedures developed by interventional radiology in the past are performed now by other physicians, eg. in the field of urology.
In this regard, it is a sign of the progress of our Society (Cardiovascular and Interventional Radiological Society of Europe), that we have been recognised as a medical specialty. This gives us more self-confidence and security. Also, I hope that this will encourage more young radiologists to join our field.
It should be emphasised that interventional radiology is a very broad field that is involved with many other (clinical) medical specialties. I think that one physician (in interventional radiology) cannot oversee and cover all interventional radiology procedures, it might be necessary to subdivide into further subspecialties. Tight cooperation and a good relationship with the colleagues of other clinical specialties is mandatory to understand the underlying disease of the patients to be treated.
Why did you choose medicine as a career, and how and why did you develop an interest in interventional radiology?
I think I was influenced as a child by my parents and their friends, who were physicians. I have always found my work exceedingly satisfying; helping sick people as a physician.
In the first year of my residency in radiology (1971), I had the chance to perform angiography, and I was fascinated by that work. Later, interventional radiology developed far beyond angiographic procedures. I enjoy working closely with patients, for me this is more satisfying than pure film or monitor reading, and this is possible with interventional radiology.
Interventional radiology has also allowed me to combine my interests in technique and physics while working with patients. This helped me to develop new medical instruments and devices.
Who have been your greatest influences?
In 1971/1972 at Johns Hopkins Hospital, EA James and Robert White motivated me most to perform experimental radiology and academic medicine. Back at Freiburg University Clinics, Germany, W Wenz and FJ Roth continued my education in angiography. At that time (1972–1978), we participated in the development of vascular interventional radiology with balloon percutaneous transluminal angioplasty and tumour embolization.
What innovations have shaped your career?
I think that the invention of stents and related developments have been the most important innovations for my career. After testing the first stent in animal experiments in Freiburg starting in 1985, together with my doctoral candidate, Beate Schneider, I implanted the first stent in a patient with a post- PTA restenosis of the right common iliac artery in May 1987.
In cooperation with Boston Scientific BSCI, we delivered the first bare-metal stent to the market in 1989. This balloon-expandable stent invented by me was knitted of a tantalum thread. Because of the material’s appropriate mechanical properties offering good stent flexibility, it was the leading vascular stent on the market for a long time. The corresponding self-expanding knitted stent design, also one of my inventions, was made of a nitinol wire, I think this was the first nitinol stent; it is mainly used for malignant gastrointestinal strictures. This stent is still highly appreciated and the leading stent for gastrointestinal and respiratory tract.
Stents opened a wide field for experimental research. So I performed the first experiments with drug-eluting stents for prevention of in-stent stenosis due to intimal hyperplasia. This was in cooperation with the Department of Pharmaceutical Technology of the University Heidelberg/Germany and the Department of Physiology of the University Tuebingen/Germany.
Together with D Liermann, I performed the first arterial intravascular brachytherapy to fight in-stent stenosis. Further, I designed stents as intravascular Can you share some of the proudest moments in your career?
I am proud of the contribution I have made to the field of interventional radiology and minimally invasive medicine.
I demonstrated that it is possible to design new medical instruments and implants with simple tools, which were principally available in the warehouse. I think it is very important to be creative in interventional radiology. Then it is possible to develop an idea and to follow it until it becomes a product.
Success does not necessarily depend on big institutions and companies, research can be performed in many places; it depends more likely on creativity, patience, and the capability to motivate other people to join your ideas and to support you.
Finally, I am proud to see that the stent idea has been accepted by so many physicians, and to see that I contributed with others to the improvement and the change of treatment procedures for vascular and gastrointestinal tract disease.
Which developing technologies or techniques in interventional radiology are you watching closely in the future?
I think the development of stent therapy is not yet finished. One of the main problems is in-stent stenosis caused by intimal hyperplasia in vascular disease, and by granulation tissue in the GI tract. I am now following new ideas to treat these entities with drug elution from stents and balloons, and the introduction of nanoparticles and stem cell therapy into this field. I am also interested in the new developments in interventional oncology.
What are the current problems/challenges facing interventional radiology?
Importantly, there is a shortage of young physicians going into interventional radiology; I hope this will change with our new status as a recognised medical specialty.
Then we have to be vigilant in the education of interventional radiologists. CIRSE has proposed three years of general radiology and two years for specialisation in interventions. Thus, within a period of five years a radiology resident could be a fully educated radiologist, which includes specialty in interventional radiology.
Also, interventional radiologists should maintain their position. Many procedures have been developed by radiologists, but people from other fields have taken over our work. I think that this is great insecurity and that it destroys a good atmosphere.
What are your current areas of research? What innovative projects are you working with?
I am trying to improve the platform of femoropopliteal stents. These should accommodate better to the anatomy and movement of the arteries. I am also developing stents for arterial bifurcations and trying to improve the systems with regard to more accurate deployment.
How do you keep up with this fast-developing field?
While it is true that IR is developing very fast, there are also many media that help to keep up with this fast development. Apart from the IR journals and IR meetings, there is the opportunity to use the internet. It is worthwhile to watch the TCT and PCR information because cardiologists have many problems with coronary arteries which are very similar to those we have with peripheral arteries. In addition, there are many basic research projects done by cardiologists from which we can transfer results to our projects.
It has become necessary to cooperate with other researchers from the field of biology, or with IT companies for further stent developments. In case you have an interesting project you will find support from other specialists.
Outside of medicine, what interests do you have?
I dedicate my time to my family. My interests include jogging, cycling and swimming. And as I am interested in science, I have started as a guest auditor to study astronomy at the University Heidelberg/Germany.
Fact File
Education and employment
1962–1968 Medical schools: Berlin, Wien, Heidelberg
Internships at the University Clinics of Lübeck, Berlin and Heidelberg/Germany
Medical degree and doctorate thesis at the University of Heidelberg/Germany in 1968
1970–1971 Training in radiology: Resident at Rhode Island Hospital, Providence/USA
1971–1972 Research Fellow at Johns Hopkins University, Baltimore/USA
1972–1978 Radiologist at the University Clinics Freiburg/Germany
1976 Residency in 1976 at the University of Freiburg.
1978–2007 Chief physician at the clinic for imaging,radiology, interventional radiology, and nuclear medicine at the Diakonissenkrankenhaus
Karlsruhe-Rueppurr Teaching Hospital of
the University of Freiburg/Germany.
Since 1982 Professor of radiology, University Freiburg/Germany
Since 2008 Consultant radiologist in Siloah Hospital Pforzheim, Germany.
Until 2009 Visiting professor in Asan Medical Centre, Department of interventional radiology, Seoul /Korea
Publications and awards
More than 300 publications in the literature, mostly in English, including chapters for books and peer-reviewed original scientific articles.
- Boris-Rajewsky Medal, European Roentgen Society, 1980
- Andreas Grüntzig Lecturer, Grüntzig Medal CIRSE, 2004
- CVIR Editors Medal 2005, CIRSE
Special scientific and technical developments
- Development of an experimental model for communicating hydrocephalus, in cooperation with AE James, MD
- Development of a mathematical model for mesenteric perfusion (Mesentericography)
- Development of an infusion pump for contrast media for small and large intestine examinations
- Experiments with MRT, in cooperation with the Bruker Company Karlsruhe, 1980.
- Development and invention of the Strecker stent 1986, first stent worldwide on the market, 1989
- First experiments with drug eluting stents and first clinical studies, 1990/1991
- Development of a percutaneously implantable catheter port system for regional arterial chemotherapy, 1990
- Development of a stent releasing system with a string to be unravelled, used for gastrointestinal and respiratory stents and stent grafts
- Development of a balloon stent graft for aortic aneurysms
- Development of different braided and knitted stent designs
- Development of a percutaneously implantable valve system
- Development of a double coil stent design
- Development of a Meander coil stent design
- Development of a double coil-membrane design for aortic aneurysm exclusion
Current research interests:
Endovascular management of aneurysmal disease, in-stent restenosis and restenosis, femoro-popliteal artery disease.












