
Reto Bale (Medizinische Universität Innsbruck, Innsbruck, Austria) gave a presentation titled ‘Stereotactic thermal ablation—can it break the current limits?’ at the 2022 European Conference of Interventional Oncology (ECIO; 24–27 April, Vienna, Austria). A key takeaway was that although the 3D planning and other elements of the stereotactic procedure may require more effort than conventional ultrasound (US)- and computed tomography (CT)-guided ablation approaches, the results that it yields are “excellent.“
His presentation covered an explanation of stereotactic thermal ablation, the logistical challenges of implementing it, and the outcomes it can achieve. Bale underlined to Interventional News that “interventional oncology must become reliable and reproducible,” and that this is what underpins the stereotactic approach.
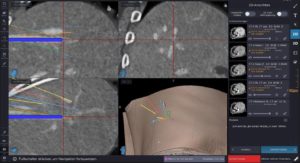
Bale’s stereotaxy workflow, he detailed, begins with “precise planning of multiple overlapping ablation zones”, to determine isotherms and to cover the whole tumour plus a safety margin. The next step, Bale relayed, is to place needles/probes in accordance with the plan, using respiratory triggering.

Bale expanded on his previous explanation, conveying how a stereotactic approach is key when dealing with tumours greater than three centimetres, as, larger than this, and ablation from a single-probe position may not be possible, hence the need for multiple needles, and the careful 3D planning that precedes their use.
Since his very first stereotactic radiofrequency ablation (SRFA) in 2001, Bale has used the image fusion software of the stereotactic navigation system to superimpose the intraoperative contrast-enhanced control CT to the planning CT for verification of complete coverage of the tumour by the ablation zone. With regard to obtaining the results of the procedure, image fusion enables the interventional radiologist to see the results of stereotactic thermal ablation before the patient even wakes up. This intraoperative verification is an advantage that stereotaxy has over radiation therapy, which necessitates waiting until long-term follow-up imaging has been completed.

Speaking to the outcomes of treating his patients with stereotactic thermal ablation, Bale stated that they very obviously demonstrate how “the additional efforts” necessary in order to conduct 3D planning, stereotactic needle placement and image fusion “lead to excellent results”. He expanded upon this assertion, explaining that his team treated more than 3,500 tumours in this way between 2001 and 2020, in more than 1,100 patients, and that even patients with multiple lesions and lesions greater than 10cm respond well. The complication rate after 2011, Bale underlines, was 0.5% mortality and 6% major complications. Of particular note is that more than half of these major complications “could be treated in the same session by the interventional radiologist.” The same is true when treating multiple lesions—they can often be treated simultaneously, in a single session.
Referencing histopathological evidence of the treatment’s success, Bale acknowledged the results of his study, which evaluated 188 hepatocellular carcinomas (HCCs) in 96 patients—the residual tumour rate was 2.7%. In lesions greater than three centimetres, the residual tumour rate is still as low as 3.8%, Bale added.
Consequently, Bale concluded, SRFA is now regarded the first-line treatment by the Innsbruck Tumour Board for most patients with primary and secondary liver tumours, encouraging clinicians first to ask themselves whether ablation could be an alternative to resection in HCC and colorectal liver metastasis patients. The advantages of the additional use of stereotaxy and image fusion are that it enables the interventional radiologist to treat more patients more consistently, with curative intent, minimally invasively, and while sparing tissue. Moreover “the beauty of the technique,” Bale emphasised, that “it is easy to teach” and that “training of three-dimensional needle trajectory planning can be done in your own lab on virtual patient datasets.”

The logistical obstacles that stand in the way of more widespread current rollout of the treatment, Bale concedes, are the need for general anaesthesia, more than three hours per patient in the CT suite, the stereotactic neuronavigation system, and “there is still a problem, also, with reimbursement.”
Bale left the audience on the note that he hopes his excellent results will encourage those responsible for reimbursement guidelines to make changes to improve the accessibility of SRFA.
A video of the procedure can be viewed here.













