Shockwave Medical has announced positive clinical results from the pooled DISRUPT PAD study, a single-arm, two-phase, multicentre study evaluating the safety and performance of the company’s Lithoplasty system in calcified peripheral lesions. The data were presented at Vascular Intervention Advances (VIVA) 2016 meeting (18–22 September, Las Vegas, USA). “The ongoing positive results from DISRUPT PAD demonstrate that Lithoplasty technology is a promising treatment for patients with calcified peripheral artery disease, a difficult-to-treat population”
The results from 95 patients with symptomatic femoropopliteal lesions up to 15cm in length enrolled at 11 sites were presented at the VIVA 16 meeting in Las Vegas, USA, by principal investigator Thomas Zeller, head of the Department of Angiology, Universitäts-Herzzentrum Freiburg, Bad, Krozingen, Germany.
The DISRUPT PAD study primary safety endpoint was freedom from major adverse events through 30 days. Procedural success, the primary performance endpoint, was defined as less than 50% residual diameter stenosis, with or without adjunctive balloon angioplasty therapy. Key secondary endpoints include target lesion revascularisation, target lesion patency by duplex ultrasound defined as freedom from greater than 50% restenosis, and functional outcomes.
“The ongoing positive results from DISRUPT PAD demonstrate that lithoplasty technology is a promising treatment for patients with calcified peripheral artery disease, a difficult-to-treat population,” said Zeller. “After six months of follow up, we have documented consistent and predictable procedural success, high acute gain, minimal vessel injury, and remarkably low need for additional implants.”
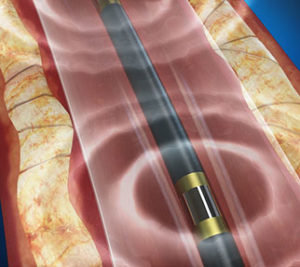
Clinical data from the study demonstrate compelling safety with no major amputations, perforations, thrombus or distal embolization events. Stent utilisation due to a flow limiting dissection following lithoplasty was limited to 1% in study population composed of moderate or severely calcified lesions. Primary effectiveness results demonstrated 100% procedural success, defined as residual stenosis <50%. An exploratory endpoint of procedural success defined as residual stenosis ≤30% was achieved in 89.5% of lesions, with an average residual stenosis of 24% and acute gain of 3mm (average RVD of 5.5 mm). Six-month patency assessed by duplex ultrasound was 77% with target lesion revascularisation of 3.2%. Over half of all patients with peripheral vascular disease have moderate or severe calcium in their arteries. Unfortunately, limitations of currently available interventional devices make successful treatment of patients with calcified arteries increasingly more difficult. The most advanced of these devices targets only superficial calcium, leaving deep calcium unaffected, frequently resulting in poor lesion dilatation and procedural complications. Designed to overcome these limitations, Lithoplasty is a novel technology that uses pulsatile mechanical energy waves to disrupt both superficial and deep calcium while minimising soft tissue injury using an integrated balloon to dilate lesions at low pressures to restore blood flow.
The Shockwave Medical Lithoplasty System is available for sale in the USA as of September 2016. The company plans a limited US commercial release in 2017 and will initiate a global randomised trial to gather further clinical data on the benefits of Lithoplasty treatment.